Cases
The Wispr At Work: Cases Using The Wispr Digital Otoscope

History of Tympanostomy Tubes – November 21, 2024
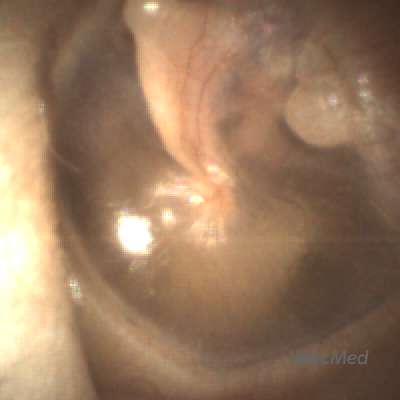
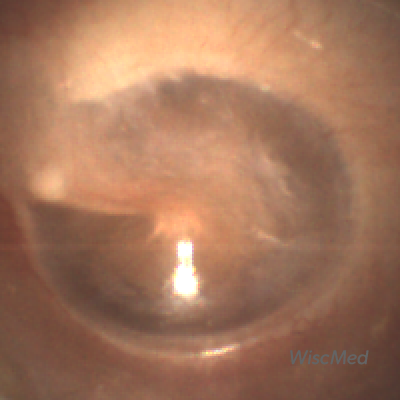
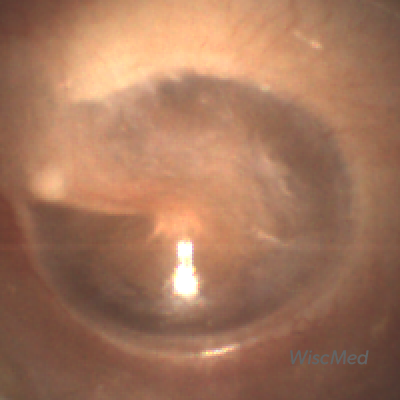
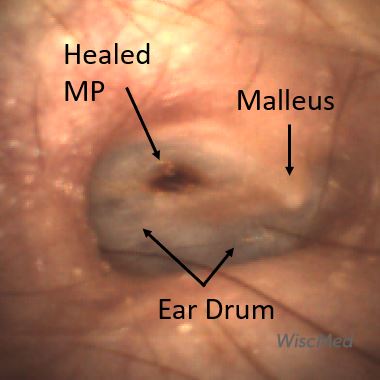
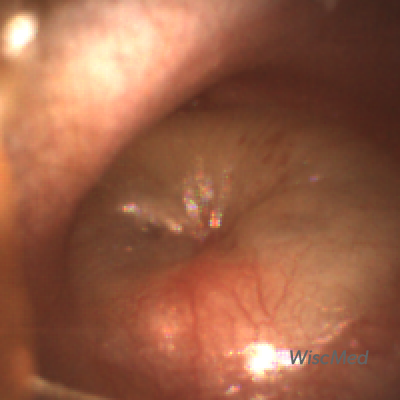
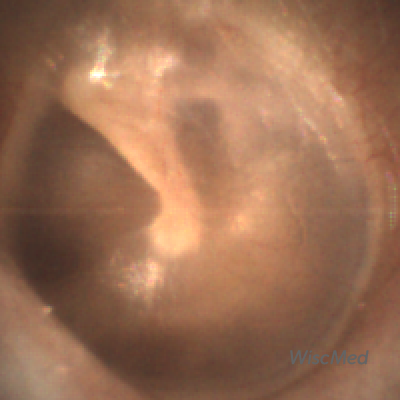
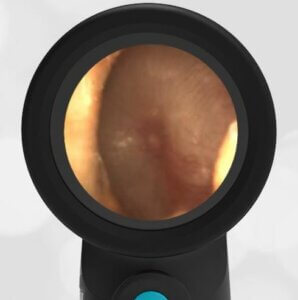
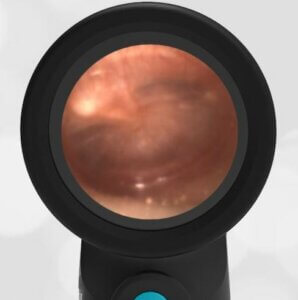
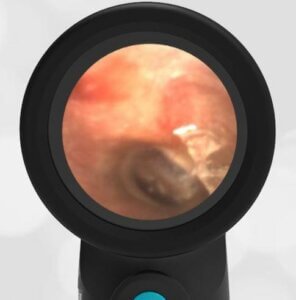
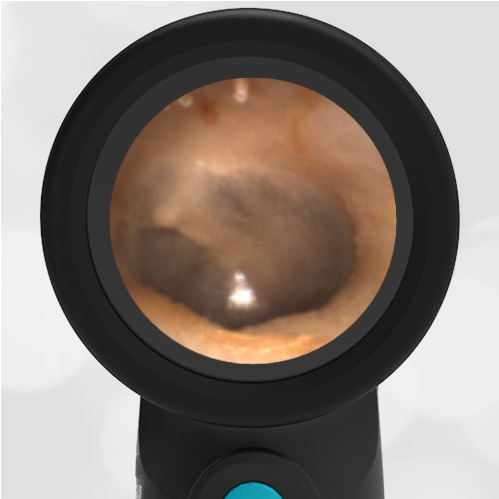
A 17-year-old male presents to the emergency department with foot pain. As part of a complete physical examination, this image of his right eardrum is obtained using the Wispr Digital Otoscope. He has no ear or hearing complaints. What caused the circular pattern seen in the inferior-anterior portion of the eardrum?
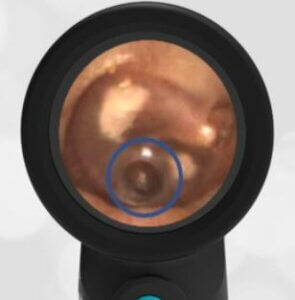
The circular defect in the ear drum (blue circled area) appears almost like a “punch biopsy.” It’s not clear what caused this pattern. An initial thought is that it is from a history of ventilation tubes (ear tubes, tympanostomy tubes). However, that seems unlikely as tube placement is accomplished by a linear incision in the ear drum which would not leave a circular pattern. From the presence of the sclerosis (white plaque), the patient has either had ear infections or ear tubes in the past.
Ear tubes are often placed in children who have recurrent ear infections. Read our prior Interesting Image on tympanostomy tubes. The ear tubes eventually fall out. After the eardrum heals, there can be evidence of the prior placement (sclerosis), as in this image.
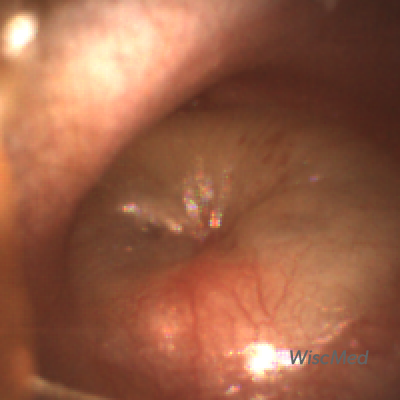
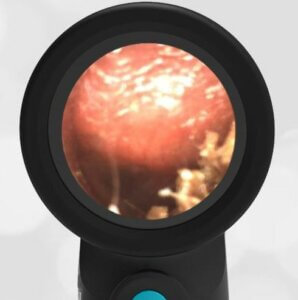
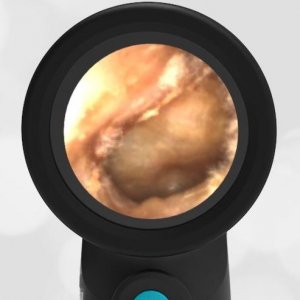
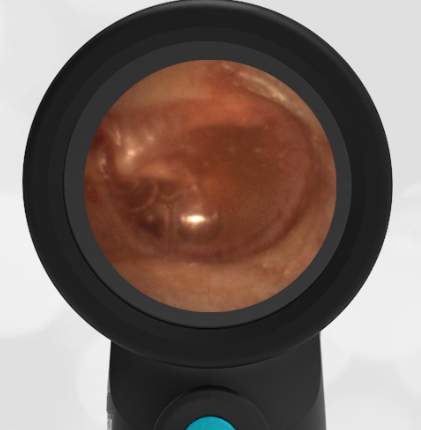
The patient’s left ear had a similar finding of post-tympanostomy tube healing and sclerosis as seen in this image:

Patient’s left ear
Key learning points
- Tympanostomy (ear tubes) are commonly placed in children who have recurrent ear infections. The tubes drain effusion from the middle ear space and equalize pressure across the ear drum.
- The placement of ear tubes often leads to patches of sclerosis on the ear drum. These have little clinical significance.
- Tympanostomy tubes fall out on their own after about 6 months and the ear drum heals.

Hemotympanum – November 14, 2024
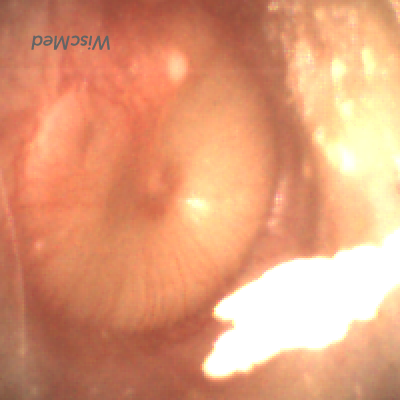
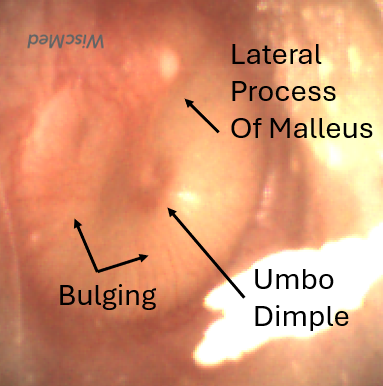
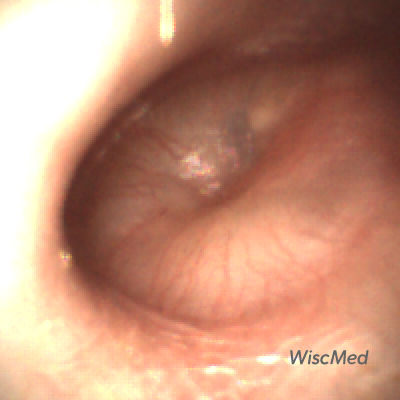
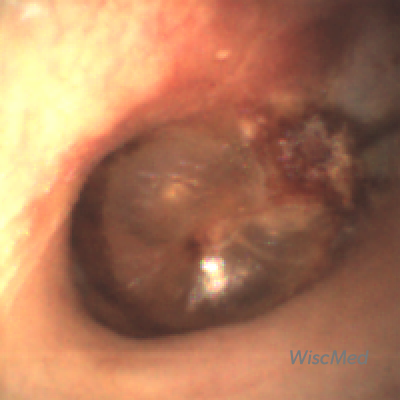
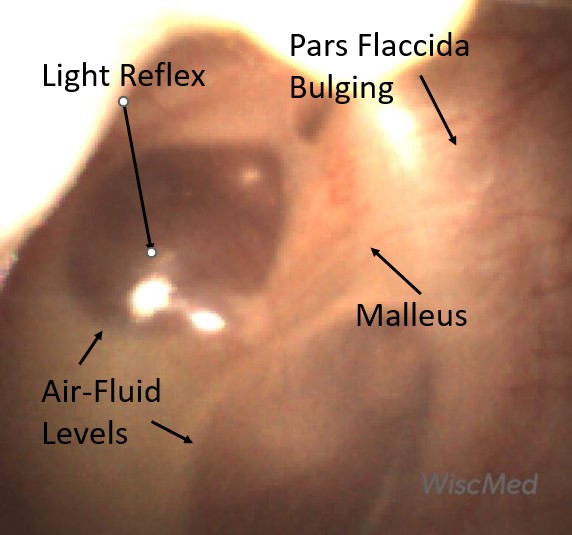
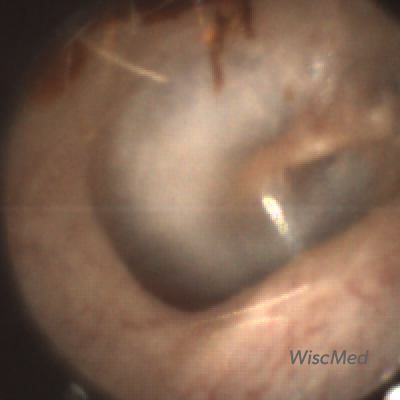
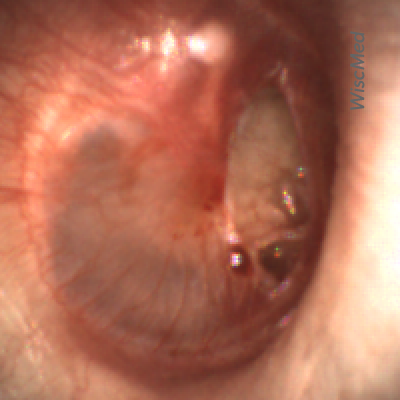
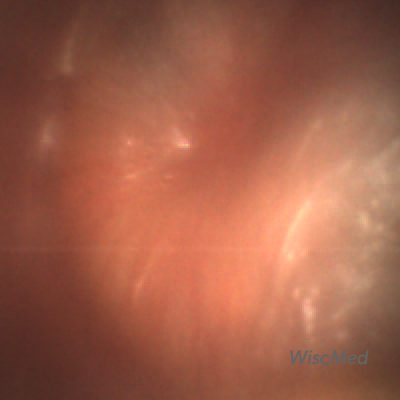
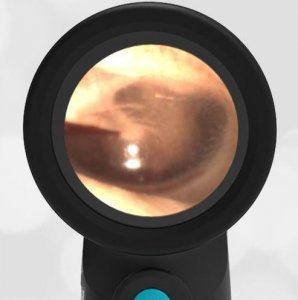
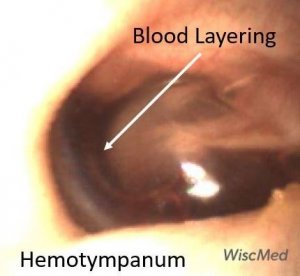
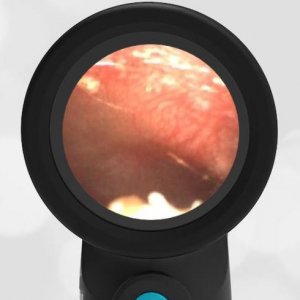
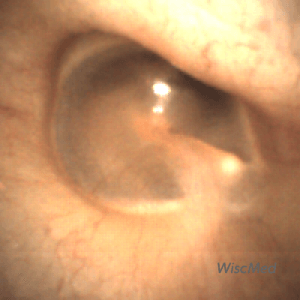
A previously healthy 3-year-old female presented to the ED for a head injury. The child was being carried by her father when he accidentally tripped and fell forward. The back of the child’s head struck the cement sidewalk—reportedly quite forcefully. However, there was no LOC, altered mental status, or vomiting. The child complained of a headache but otherwise had no other symptoms. The parents felt that “she appeared normal” to them but brought her in for evaluation because of the headache. On examination, the child was smiling, and interactive and had no swelling, step-offs, or other deformities to her head. She had an entirely normal neurologic examination. Wispr examination revealed this image.
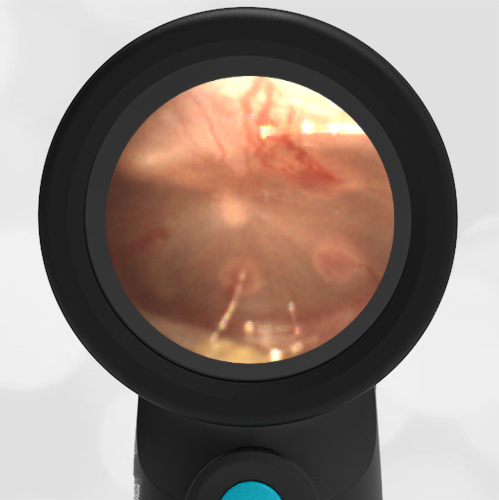
This child’s Wispr examination demonstrates a darkened, bulging TM consistent with hemotympanum (blood behind the ear drum).
In the setting of head trauma, the hemotympanum typically occurs as a result of a basilar (lower) skull fracture with subsequent bleeding into the middle ear space.
Hemotympanum is often the earliest sign of basilar injury. Other later physical exam findings may include “raccoon eyes,” and bruising behind the ear. Despite the child’s well-appearance (she was deemed PECARN negative), the finding of the hemotympanum led the clinicians to pursue neuro-imaging that revealed a minimally displaced temporal bone fracture. The patient was admitted to the pediatric neurosurgery service for observation and recovered uneventfully from her injury without intervention.
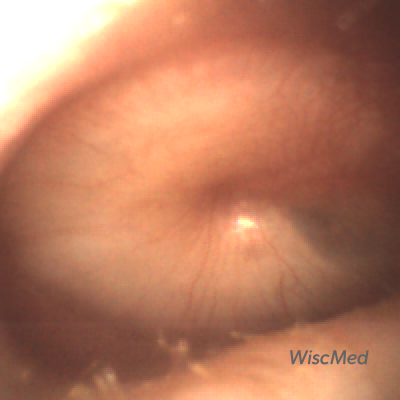
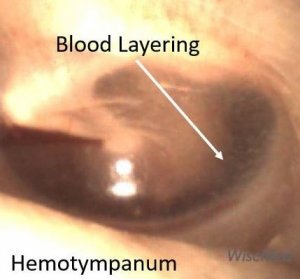
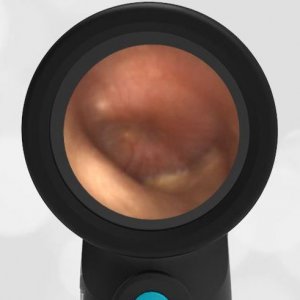
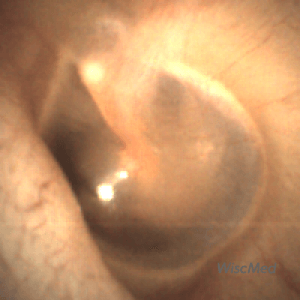
Interestingly, in this case, the initial evaluation was performed by standard otoscopy and reported as “a little dark in the canal, but otherwise normal”—a fact that demonstrates the challenge of viewing a non-perforated hemotympanum with a traditional otoscope. Light does not reflect strongly off the darkened TM which, combined with the small canal diameter and the brief view so common in pediatrics, results in an incomplete assessment of the TM. Furthermore, just as with otitis media, not all hemotympanum appear the same (see the image below from a 10-year-old child who fell from a barn loft and sustained a complicated basilar skull fracture). In both cases, the WiscMed Wispr achieved diagnostic images that assisted clinicians with the correct neurologic workup, diagnosis, and treatment.

Hemotympanum in a 10-year-old
Key learning points
-Hemotympanum is blood behind the ear drum, i.e. in the middle ear space.
-It can be caused by head injury, increased pressure in the middle ear space, or epistaxis (nose bleed) with blood flowing retrograde up the Eustachian tube to the middle ear space.
-Hemotympanum requires urgent evaluation for the source as it can indicate a serious injury. Often, advanced imaging is required.
Here is the complete video exam
Here is another case that shows bilateral hemotympanum caused by epistaxis (nosebleed).

Spring In Mouth – November 7, 2024
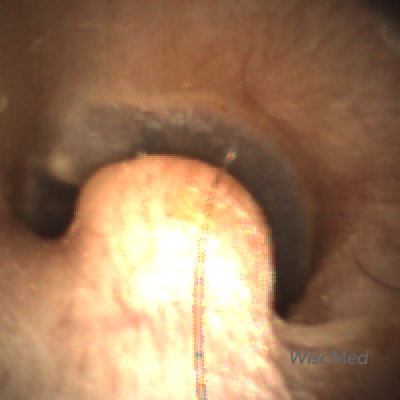
A 2-year-old male is brought into the emergency department by his grandmother for noisy breathing. The grandmother reports that the child was unsupervised in the other room “for only seconds” when she began to hear crying and then noisy breathing. Before the event, the child had been doing well, meeting all developmental milestones, and thriving with his family. The examination of the mouth with the Wispr Digital Otoscope reveals this image.
The child has a metal spring in his posterior pharynx.
Although the child was breathing noisily, his airway was patent and his oxygen saturation was normal. Because of this, removal was urgent, but not emergent. It was unknown how deeply the spring was embedded in the soft tissues of the throat, and there was concern that removing the spring could lead to trauma and a potential airway disaster. For this reason, otolaryngology (ENT) was consulted. ENT removed the spring uneventfully in the emergency department with forceps. No sedation was required.

Removed spring
Although the Wispr Digital Otoscope is optimized for visualization of the anatomy of the ear canal, it can be a useful tool in both the mouth and nose.
Key Learning Points
- Pediatric airways are small and susceptible to blockage from foreign bodies or infection.
- Don’t turn an urgent situation into an emergent situation. Get the right expertise involved.
Here is the complete video exam

Primary Blast Injury – October 31, 2024
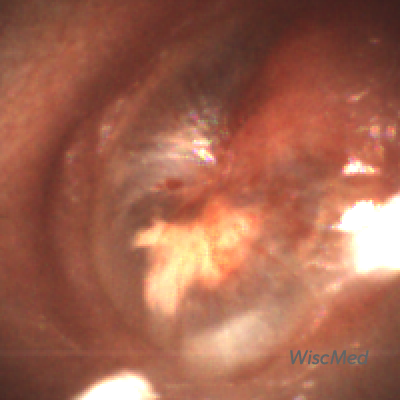
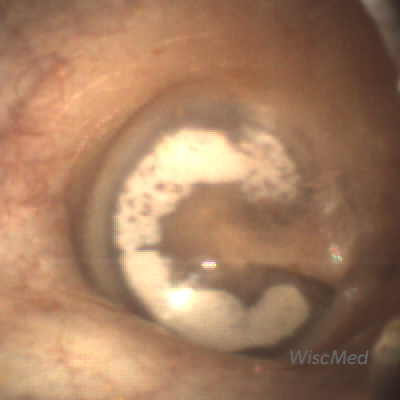
A teenager presents to the Los Angeles pediatric emergency department complaining of decreased hearing and pain in his left ear. Prior to presentation, the youth and his friends had been playing with fireworks when a large firecracker detonated close to the left side of his head. Examination of the left ear with the Wispr Digital Otoscope reveals this image.
What is the next step in management?
- Admission for emergent surgery
- Start antibiotics
- Watchful waiting with instructions to avoid water
- Urgent consult to otolaryngology (ENT)
Answer 4. Urgent consult to otolaryngology (ENT)

The teenager has suffered a primary blast injury to his eardrum.
There is a significant disruption of the tympanic membrane (eardrum) which is circled in this image.
Blast injuries are classified as follows;
- Primary – from the pressurization wave of the blast. Primary injuries present to the lung, eye, eardrum (as in this case), abdomen and brain.
- Secondary – from flying debris. Secondary injuries can occur anywhere. An example would be penetrating injury from metal that was surrounding a bomb. The individuals who were injured at the Boston Marathon bombing suffered secondary blast injuries.
- Tertiary – from the individual being thrown by the blast. Tertiary injuries present as orthopedic or traumatic brain injuries.
- Quaternary – explosion related. Examples of quaternary injuries include burns, crush injuries, asthma exacerbations from dust storms, and radiation exposure.
Minor tympanic membrane ruptures generally heal on their own. In this case, the damage is significant, clearly affecting where the malleus attaches to the tympanic membrane. This patient needs an urgent consultation with otolaryngology (ENT). The decision to start medication would be guided by a stat consult with ENT but is generally not indicated. The patient should be told to avoid any moisture in the ear until evaluated by ENT. He will likely need surgical intervention to repair the extensive damage to both the tympanic membrane and the middle ear structures.
Key Learning Points
- Tympanic membrane ruptures are common and can occur from insertion of foreign objects, blasts, and diving.
- Small ruptures often heal on their own and do not require intervention. Large or complex ruptures require ENT evaluation.
- Antibiotics are generally not indicated for a clean rupture.
- Water such as found in a pond, lake or pool should be avoided until seen by ENT.
WiscMed thanks Dr. Patricia Padlipsky of Harbor-UCLA for contributing this interesting image.
Reference

Ant in Ear Canal – Oct 24, 2024
A 7-year-old male presented to the pediatrician’s office with fever, vomiting, and diarrhea. The child was diagnosed with viral gastroenteritis. As part of the complete physical exam, the following image was obtained of his left ear with the WiscMed Wispr digital otoscope. When asked about the finding of the ant in the ear, the mother mentioned that they occasionally see ants in the house. Ten days ago, the child woke up with severe left ear pain. The mother gave ibuprofen and instilled otic ear drops. The pain was gone almost immediately.
What is the next step in management?
- Refer the child to otolaryngology (ENT) for removal
- Remove the ant with a forceps
- Remove the ant with lavage
- Remove the ant with a Q-Tip
Answer: 3. Remove the ant with lavage

A reasonable first attempt would be to remove the ant with lavage – i.e. rinse the dead ant out of the external ear canal. However, in this case, the ant was adherent to the canal wall, and the lavage was unsuccessful. Using a forceps will not work as it would likely break the dead ant into many pieces. A Q-Tip would have the same issue as a forceps. In this case, the child was referred to ENT for complete removal of the ant.
Foreign bodies in ear canals are very common. Examples include beads, tic-tacs, pencils, ticks and hearing aid tips.
Key Learning Points
- Foreign bodies in the external ear canal are common.
- Removal of the foreign body is facilitated by proper visualization.
- Removal technique depends on the nature of the foreign body.
- With a pediatric patient, you generally get one chance at removal before an ENT consult and sedation is required.
WiscMed thanks Dr. Joao Mauricio Scarpellini Campos for this interesting case. Dr. Campos is a pediatrician in private practice in Rio de Janeiro, Brazil.
Here is the complete video exam

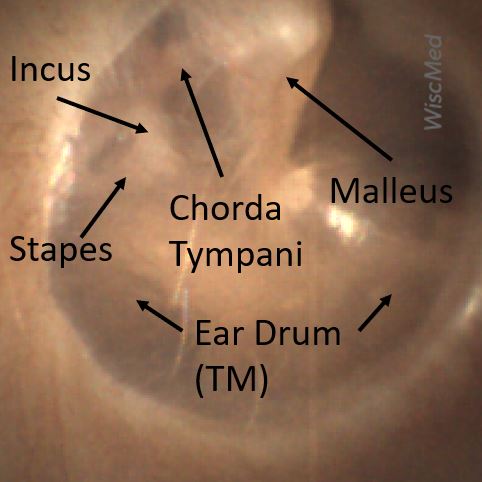
Otitis Media with Effusion – October 17, 2024
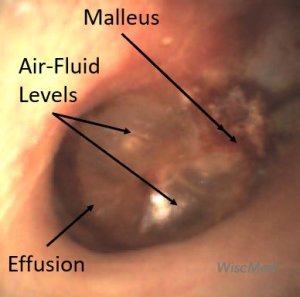
A 12-month-old female presented to the pediatric emergency department (ED) with concern for an ear infection. The mother reported a week of runny nose and mild cough as well as subjective fever. The day prior, she was putting a finger into her right ear, so she was taken to Urgent Care where she was diagnosed with an ear infection. The mother reported the child was refusing to take the “pink antibiotic”, so they came to the ED seeking an alternative. Upon evaluation, the child is afebrile with normal vital signs. She has clear nasal drainage. Auscultation revealed very mild wheezes bilaterally. The Wispr digital otoscope exam is attached below.
What is the appropriate management for this child’s condition?
- Discontinue the antibiotic and recommend supportive measures
- Continue the current antibiotic, but recommend putting it in juice or syrup to mask the taste
- Change the antibiotic to amoxicillin plus clavulanate
- Refer the child to otolaryngology (ENT) for audiometry and tympanostomy tube placement
Answer: A. Discontinue the antibiotic and recommend supportive measures

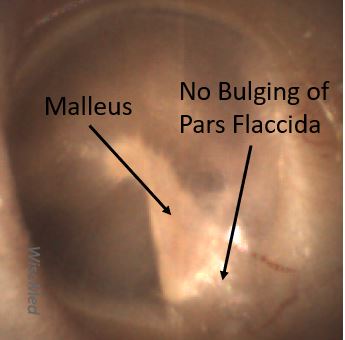
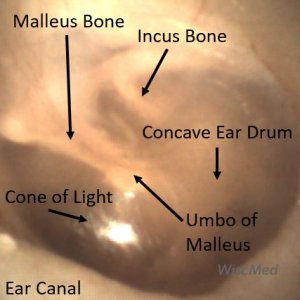
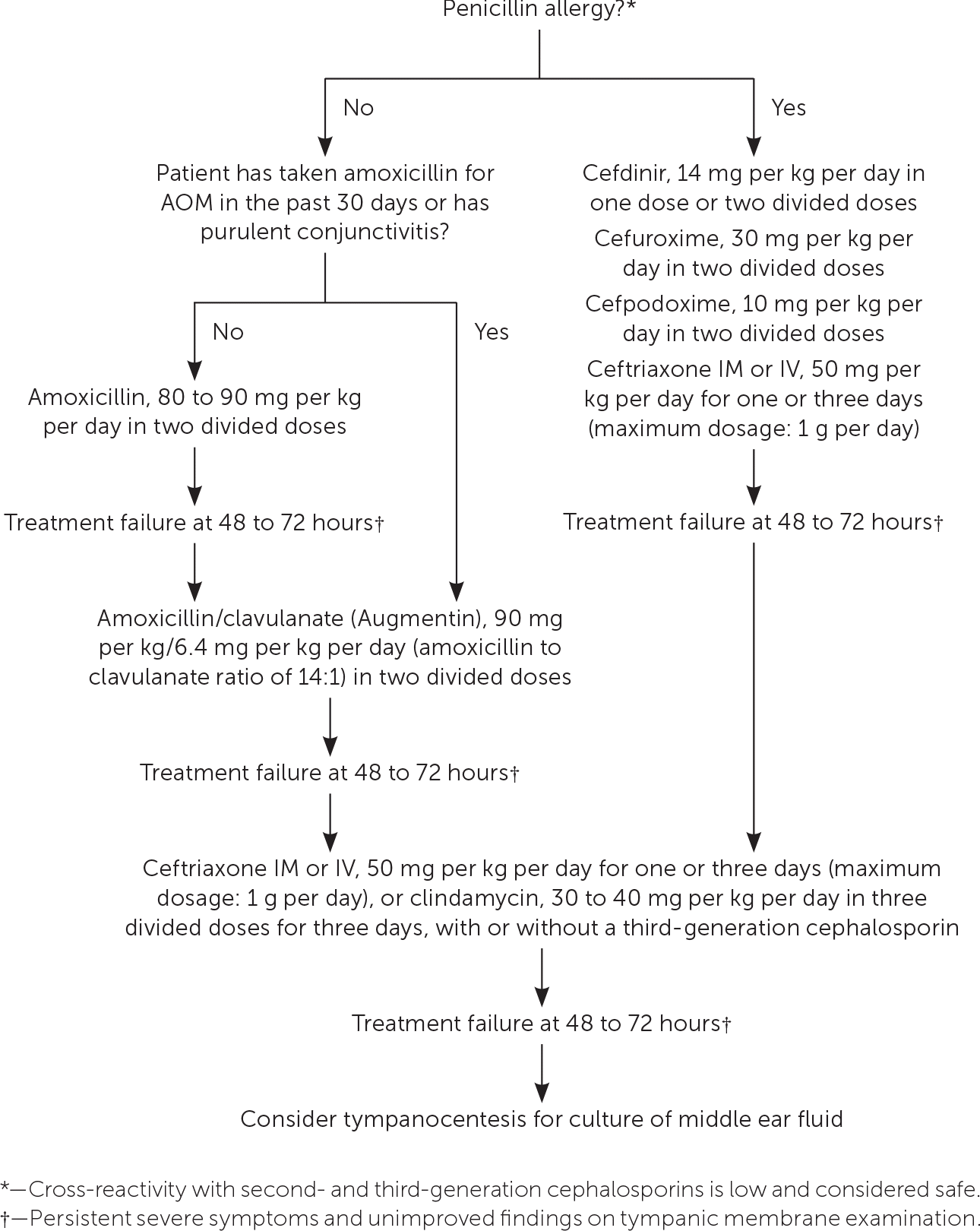
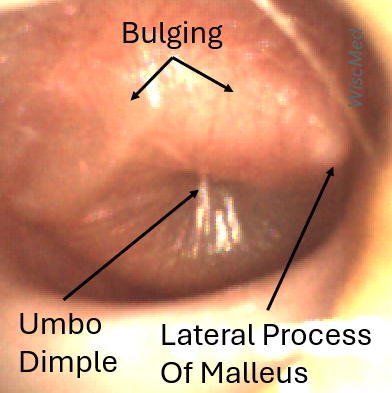
This child’s Wispr otoscope exam demonstrates a right-sided middle ear effusion (MEE) as evidenced by visible air bubbles behind a clear tympanic membrane (TM, “ear drum”). Since the child’s TM is not bulging (notice how the malleus is easily identified) nor is there marked erythema (redness), the diagnosis of Acute Otitis Media (AOM) should not be made. Therefore, her diagnosis is most consistent with Otitis Media with Effusion (OME) which does not require treatment with antibiotics. The presence of the air-fluid levels without bulging indicates that the Eustachian tube is ventilating the middle ear space appropriately.
OME is a common finding in young children with viral respiratory infections that may occur following a bout of AOM or simply because of Eustachian tube dysfunction. In both instances, the child may exhibit signs of discomfort that may incline one to overtreat as presumed AOM if the diagnosis is not certain. This case reinforces the importance of adequate visualization of the TM to avoid this pitfall. Beyond symptomatic management, referral to ENT for evaluation may be indicated if the child has risk factors for hearing loss (such as craniofacial abnormalities, known hearing deficits, or language delays) or if the OME persists beyond three months.
WiscMed has created a visual guide to common ear conditions that may be found here.
Key Learning Points
-Proper visualization of the tympanic membrane is required for any diagnosis
–Otitis Media with Effusion is characterized by air-fluid levels behind the tympanic membrane without evidence of bulging or loss of bony landmarks.
–Otitis Media with Effusion does not require antibiotics
Here is the complete video exam
Reference:

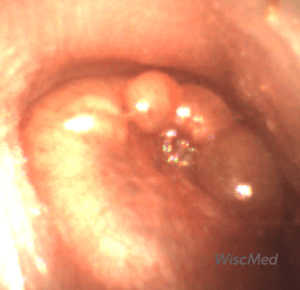
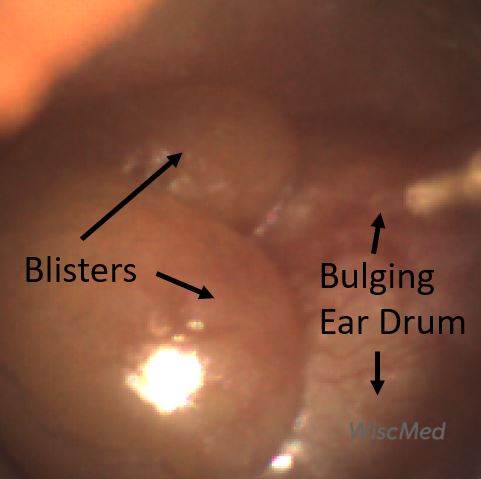
Bullous Myringitis – October 10, 2024
An 8-year-old boy presented to the Pediatric emergency department (ED) late in the evening complaining of ear pain. He had several days of mild upper respiratory symptoms but no fever or significant cough. However, he awoke that evening with severe left ear pain. It was not relieved with ibuprofen, so his mother brought the child to the ED for evaluation. He was afebrile with age-appropriate vital signs. The physical exam was remarkable for an obviously uncomfortable child, holding his left ear. His Wispr digital otoscope exam is pictured below.
Which of the following is an associated etiology of the child’s finding?
- Streptococcus pneumoniae
- Moraxella catarrhalis
- Group A Streptococcus
- Respiratory Syncytial Virus (RSV)
- All the above
Answer: E. All the above

The child’s diagnosis is bullous myringitis which is characterized by painful vesicles or bullae (blisters) on the tympanic membrane (TM). These bullae may be quite large and occasionally hemorrhagic. Common etiologies are viruses, such as RSV and influenza. However, the typical acute otitis media bacterial pathogens are also frequently associated with bullous myringitis. Streptococcus pneumoniae is the most commonly identified bacteria, followed by Moraxella catarrhalis, Group A Streptococcus, and Staphylococcus aureus. Acute otitis media (AOM) is also an infection in the middle ear space. AOM’s diagnostic hallmark is bulging of the TM without the presence of the bullae found with bullous myringitis.
WiscMed thanks Dr. Joseph Stearns of the University of Wisconsin BerbeeWalsh Department of Emergency Medicine for this case.
Here is the complete video exam
Reference:

TMJ Compression of External Ear Canal – October 3, 2024
A 41-year-old woman was given a demonstration of the WiscMed Wispr digital otoscope at the American Academy of Pediatrics national convention. She mentions that in the past year, she has had increasing discomfort of her right temporomandibular joint (TMJ). She also says that the hearing in her right ear has significantly diminished. She has had no fevers, no unexplained weight loss, and no headaches. The following image of her right ear canal is obtained.
What is the next step in management?
- Urgent consultation to otolaryngology (ENT)
- Obtain a CT scan of the temporal region
- Begin antibiotics
- Begin a course of high-dose steroids
Answer 2. Obtain a CT scan of the temporal region

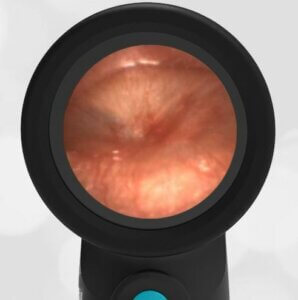
The woman has a significant occlusion of her external ear canal, likely caused by mechanical compression associated with the TMJ. Compare the image of this patient’s external canal with a normal canal. Note that a normal external canal is round while the patient’s canal is so compressed as to appear as a slit.
There is no indication of infection, i.e. no erythema or evidence of inflammation, so antibiotics are not indicated. High-dose steroids are not indicated until further information regarding the cause of the compression is determined. A CT scan or MRI would be the next step to identify the source of the compression and to eliminate the possibility of a tumor. After advanced imaging, a consult with otolaryngology would be appropriate.
The patient was asked to open her mouth widely and move her lower jaw to the left. When she did so, the external canal opened slightly, and a partial view of the tympanic membrane (ear drum) was obtained. The visible portion of the eardrum appeared healthy and normal.

Mouth open with lower jaw moved to the left.
Here are the complete videos of the exams with both the mouth closed and the mouth open with the lower jaw displaced to the left.
Mouth Closed
Mouth open, lower jaw to the left

Tick in Ear – September 26, 2024
A 63-year-old male veteran presents to the veterans affairs (VA) emergency department with concerns for painless decreased hearing in one ear. The following image is obtained.
What is the next step in management?
- Urgent consultation to otolaryngology (ENT)
- Exploration of the foreign body with forceps
- Flushing of the foreign body with saline
- Initiation of antibiotics
Answer 1. Urgent consultation to otolaryngology (ENT)
The veteran has a tick attached in his external auditory canal.

On the initial exam, the pathology shown in the image was unclear. The appearance was inconsistent with an infection such as acute otitis media (AOM). Flushing was dismissed as the object appeared attached to the eardrum or ear canal. Exploration of the foreign body with forceps was considered but dismissed based on the high risk of probing an unknown object near the ear drum. Otolaryngology (ENT) was e-consulted with this image and thought it might be a polyp. A consultation appointment with ENT was made for the veteran.
The veteran returned to the VA about a week later for a different issue. At that visit, he reported to medical staff that a fully engorged tick had crawled out of his ear the prior day.
On re-evaluation of the image, it clearly shows congealed blood adjacent to the “polyp” consistent with a tick attachment.
Here is a video of the exam with the tick present.

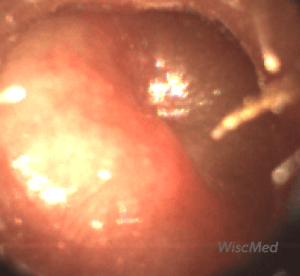
Acute Otitis Media – September 19, 2024
A 4-year-old child presented to the Pediatric emergency department (ED) with a complaint of ear pain. Her mother reported her daughter had a few days of nasal congestion and complained of pain in the right ear the previous day. She did not seek care since there was no fever and the pain resolved with ibuprofen. However, shortly after going to bed, she awoke crying due to ear pain. This time, the ibuprofen did not seem to help, so she was brought in for evaluation. In the ED, the child is febrile to 102oF. She appears uncomfortable and hesitant to allow an ear exam. With gentle coaxing, the Wispr digital otoscope exam was obtained and is shown. Her medical history is unremarkable, she has no known drug allergies and has had only one ear infection in the past. Mom did not recall how long ago, but it resolved with “the pink medicine.”
What is the appropriate management for this child?
- Ibuprofen and just-in-case prescription of antibiotics
- Treat immediately with amoxicillin and consider topical anesthetic
- Treat immediately with Augmentin
- Treat immediately with azithromycin
Answer: B. Treat immediately with amoxicillin and consider topical anesthetic

The child in this case has right acute otitis media (AOM) as evidenced by moderate bulging of the tympanic membrane (TM ). The TM is impressively injected centrally over the umbo and has a cloudy middle ear effusion (MEE). There is also a rim of cloudy MEE suggesting an evolving AOM. Since she has not received antibiotics in the previous 30 days, first-line therapy is high dose amoxicillin (40-45mg/kg twice daily). Given her level of pain has not improved with ibuprofen, treatment with a topical anesthetic such as proparacaine drops may be considered for more immediate relief of symptoms.
WiscMed has created a visual guide to ear diagnosis that can be found here.
Here is the complete video exam.
Reference:
Allan S. Lieberthal, Aaron E. Carroll, Tasnee Chonmaitree, Theodore G. Ganiats, Alejandro Hoberman, Mary Anne Jackson, Mark D. Joffe, Donald T. Miller, Richard M. Rosenfeld, Xavier D. Sevilla, Richard H. Schwartz, Pauline A. Thomas, David E. Tunkel; The Diagnosis and Management of Acute Otitis Media. Pediatrics March 2013; 131 (3): e964–e999. 10.1542/peds.2012-3488

Myringosclerosis – September 12, 2024
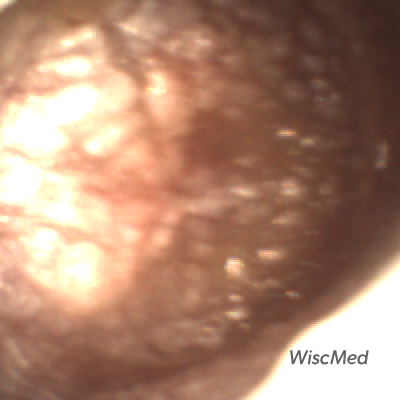
A 28-year-old medical student beginning her emergency department (ED) rotation agreed to have her ears examined during otoscopy training. She reports excellent hearing and is in good health.
Her Wispr digital otoscope exam is shown.
Which of the following is likely to be true of her medical history?
- She had frequent exposure to cold water
- She had myringotomy (ear) tubes placed as a young child
- She had surgery to remove a cholesteatoma
- She has had barotrauma
Answer: 2. She had myringotomy (ear) tubes placed as a young child

The Wispr exam reveals impressive myringosclerosis. Myringosclerosis is a build-up of calcium in between the tympanic membrane (TM) layers and is typically asymptomatic without impacting hearing. This contrasts with tympanosclerosis in which calcium deposition also occurs in the middle ear space and may result in conductive hearing deficits. The most common causes of both conditions include recurrent acute otitis media, chronic otitis media with effusion, and surgical placement of myringotomy (ear, ventilation) tubes.
Frequent exposure to cold water results in exostosis, commonly called “surfer’s ear.” A cholesteatoma is a benign growth in the middle ear space that can erode the ossicles and cause hearing loss. The malleus shown in this image is the first of three middle ear ossicles. Baro trauma such as from an explosion causes a rupture in the tympanic membrane. The yellowish-appearing blob in the image is ear wax, known as cerumen.
The medical student in this vignette confirmed her history of recurrent AOM and myringotomy tube placement as a child. She also took images of her tympanic membranes to send to her mother, who she felt would be thrilled to see what she is learning on her Emergency Medicine rotation.
Here is the complete video exam.

Mud Spots or Resolving Middle Ear Muco-Purulence (REMEMP) – September 5, 2024
An 18-month-old female presents for a re-evaluation of her left ear. Twelve days prior the child was diagnosed with acute otitis media (AOM) and placed on antibiotics. The child’s symptoms improved immediately, and today the mother has no further concerns. The follow-up exam was done as an academic exercise to track the resolution of AOM.
What abnormalities do you note in the image obtained of the left ear?
There are several abnormalities still present on the left ear tympanic membrane (TM). The malleus, while discernable, still does not appear as distinctly as in a normal ear. The pars flaccida portion of the TM still shows signs of mild bulging. There is subtle shagrination present. Most interesting, perhaps, is the presence of the “mud spot.” Mud spots are well described in Chapter 9 of Dr. Michael Poole’s excellent book, “Otitis: The Expert’s Diagnostic Guide.” Mud spots are often found in cases of resolving acute otitis media. They are typically seen from one to eight weeks after AOM and are located on the medial surface (middle ear surface) of the TM.
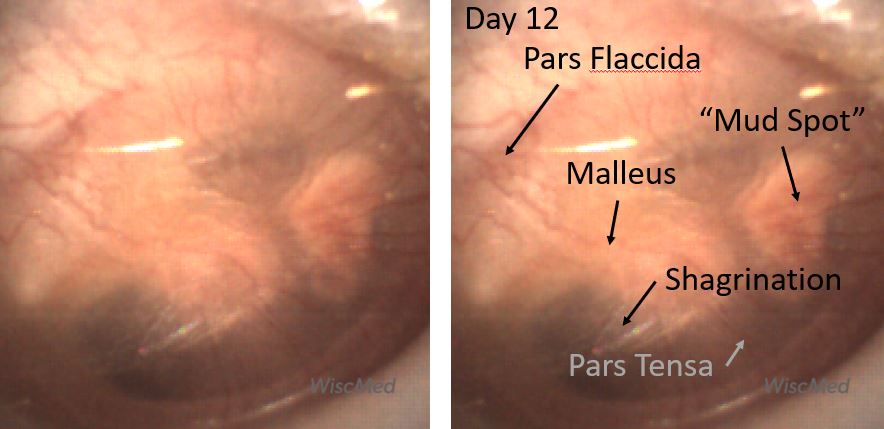
Day 12 post-AOM diagnosis and treatment
Mud spots are thought to be from the aggregation of inflammatory cells secondary to the resolving infection. The spots resolve with time as can be seen in the panels below. The mud spots appear to resolve more quickly if there is no middle ear effusion present. Dr. Poole has introduced the term Resolving Middle Ear Muco-Purulence (REMEMP) as a more academic term than mud spots. The following three panels show the tympanic membrane prior to the mud spot developing (day 9), the presence of the mud spot (day 12, this case), and resolving of the mud spot (day 25).

Day 9 post AOM diagnosis and treatment with developing mud spot
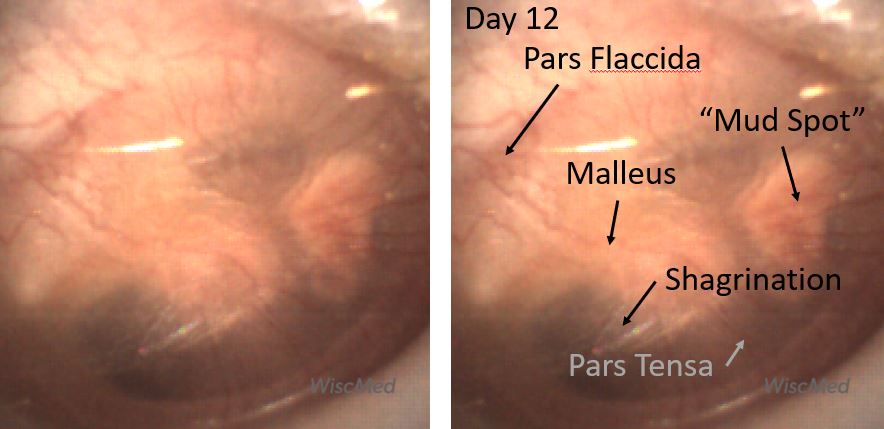
Day 12 post-AOM diagnosis with formed mud spot
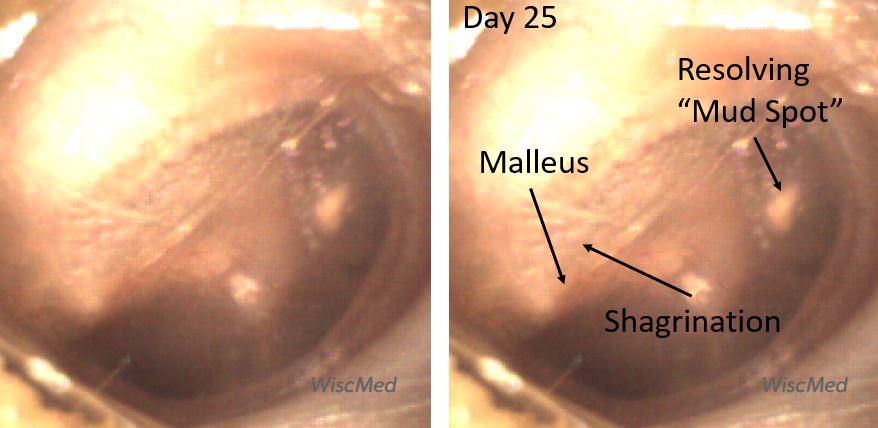
Day 25 post-AOM diagnosis with resolving mud spot
Here is the complete video of the day 12 ear exam:
Reference
“Otitis: The Expert’s Diagnostic Guide,” Dr. Michael Poole, Apple Books.

Ear Wax – August 29, 2024
A 9-year-old female presents to the general pediatric clinic in the summer for a routine checkup. She has no specific complaints. Examination of the right ear with the Wispr Digital Otoscope reveals this image.
What is the next step in management?
- No action is necessary, the ear is normal.
- A better view of the ear drum should be obtained.
- Begin a course of antibiotics for otitis externa.
- Referral to otolaryngology (ENT)
Answer: B. A better view of the ear drum should be obtained.
The image shows only cerumen (ear wax). It is not possible to form an opinion of the eardrum, normal or not, from this image. This view is often seen with traditional analog otoscopy – that is, nothing is seen but wax that is occluding the eardrum and preventing evaluation. Otitis externa (swimmer’s ear) can look like cerumen. However, with otitis externa, there would be symptoms such as ear pain. The patient in this vignette has no symptoms to suggest otitis externa.
Because of the unique geometry of the WiscMed Wispr speculum combined with the distally mounted camera, it is often possible to maneuver around the ear wax and obtain a view of the eardrum. Here is a still image of the normal eardrum after using the Wispr to navigate past the wax.

This ability of the Wispr Digital Otoscope to maneuver around wax may increase the speed and comfort of the examination as there is often no requirement to remove ear wax. Here is a video showing this technique with the Wispr.

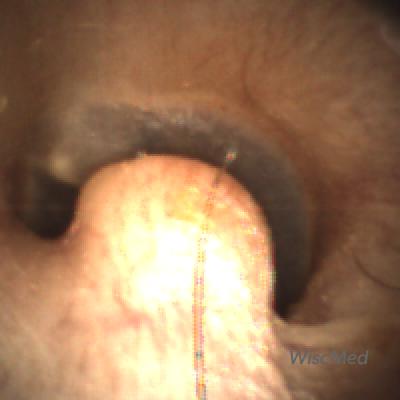
Bilateral Osteoma – August 22, 2024
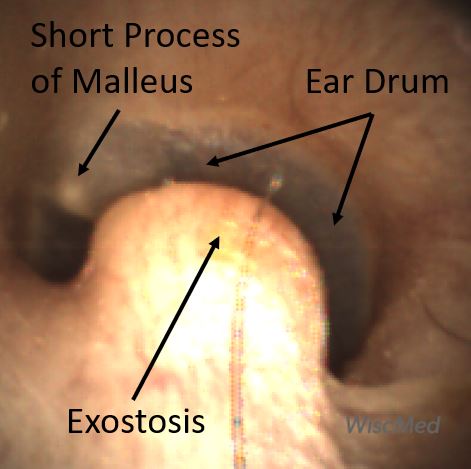
An active 36-year-old male presents to the emergency department for a concern unrelated to his ears. However, his Wispr digital otoscopic ear exam reveals an interesting finding.
Which of the following is most likely the patient’s favorite pastime?
- Diving
- Mountaineering
- Surfing
- No indication from this image
Answer 4. No indication from this image.

The patient has an osteoma in his external ear canal (EAC). An osteoma is a benign bony neoplasm with no specific cause. Osteomas are generally single, unilateral, and have a pedunculated base while exostoses are often multiple, bilateral, and have a wider base. An osteoma can be easily confused with an exostosis, the other common lesion found in the EAC. Exostosis is associated with exposure to cold water such as from surfing. Diving is associated with ear trauma such as perforation. Mountaineering is not associated with any specific ear finding although Eustachian tube dysfunction can cause an uncomfortable sensation, like ear popping during descent in an airplane.
The two growths can be difficult to distinguish in mild cases by appearance alone. However, they are histologically distinct with exostoses having a laminated appearance representing layers of newly formed bone. This is believed to occur when repeated exposure to cold water triggers periostitis resulting in sequential episodes of osteogenesis, giving rise to the term “surfer’s ear.” Osteomas arise from cancellous bone and lack the layered growth pattern of exostoses. Both lesions are generally asymptomatic unless they enlarge enough to cause conductive hearing loss. In these instances, referral to otolaryngology (ENT) is warranted for further evaluation and potential surgical removal.
Although osteomas are generally unilateral, this patient had evidence of osteomas in both ears.
Reference
Here are the video exams from the Wispr otoscope of both ears:
|
Left Ear Video |
Right Ear Video |

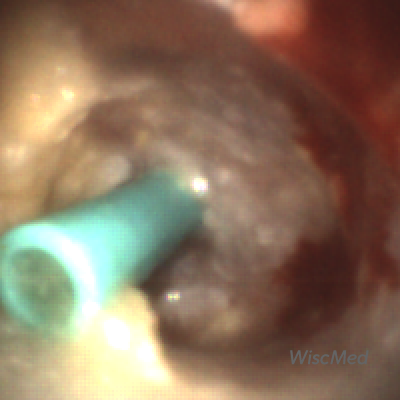
Foreign Body – August 15, 2024
An 8-year-old presented to the emergency department (ED) for a foreign body in her ear. The child states she placed an “orbeez” water bead in her ear while she was visiting her family four days prior. She spent the weekend swimming and being otherwise active. When she returned home, the child told her mother about the foreign body who attempted to remove it without success. She was not complaining of any pain, but her hearing was muffled. In the ED, she was a talkative and obviously curious child. Her Wispr digital otoscope exam is shown.

This child presented for an ear foreign body that was successfully and painlessly removed with a small suction catheter, facilitated by direct visualization with the Wispr digital otoscope. The video removal of the bead is shown below.
Water beads are tiny soft polymer spheres that expand massively when placed in liquids. Pediatric complications related to ingestion or placement in the external auditory canal (EAC) are common and have been implicated in serious injury. Tragically, there have been two reported deaths following ingestion in toddlers. When dry, these beads are only several millimeters in diameter and thus can be easily ingested or placed into the ear canal. However, shortly after becoming moist or immersed in liquid, they begin to expand and may reach 100x the initial diameter.
The child in this case is fortunate to have had such an uneventful foreign body retrieval. In a 2023 case series of seven children presenting with water beads in the ear, six required removal under general anesthesia with three needing additional surgical intervention to restore hearing deficits. In the most severe case, the bead had been present for months, undetected despite multiple visits to the ED for drainage, pain, and decreased hearing. This case is a reminder that children can and will put anything that fits into their ear, nose, and mouth–early recognition and management are important, particularly when water beads are suspected!
Children are well-known for placing foreign bodies in their ears. Examples include tic tacs, pencils, beads, and beans.
WiscMed thanks Dr. Michael Kim of the University of Wisconsin – Madison BerbeeWalsh Department of Emergency Medicine for this week’s interesting case.
Here is the complete video.
References:

Ant in Ear – August 8, 2024
A 12-year-old male, the son of a pediatrician, complains of something tickling his ear. The patient has no history of ear infections or trauma. He had been playing out in the yard. The image of the patient’s right ear is shown.
What’s the next step in management?
- Urgent consult to otolaryngology (ENT)
- Foreign body removal with forceps
- Watchful waiting with careful return instructions
- Flush the foreign body using a syringe
Answer D. Flush the foreign body using a syringe
The child has a live ant in his external auditory canal (EAC). The sensation of a bug moving in the EAC is distressing. For patient comfort, the foreign body needs to be removed. A consult to ENT without first trying to remove the object in the clinic would not be appropriate. Trying to grab a moving object with a forceps would be difficult. It is also likely to lead to ant debris in the canal. The best answer is flushing the foreign body using a syringe. That was done in this case, and the ant was easily removed. It’s unknown if the ant survived the procedure.
Foreign bodies in the ear canal are common. Examples include flies, tic tacs, pencils, spiders, beans, and beads. The removal technique depends on the type of foreign body. Common techniques include flushing, forceps, Katz extractor, glue stick, and suction. With pediatric patients, the clinician generally has one chance to remove the foreign body before the patient becomes uncooperative and sedation is required. A benefit of the Wispr digital otoscope is the ability to visualize the foreign body and plan for the best removal technique.
Here is the complete video exam:
WiscMed thanks Dr. Neil Cella of Care Point Health Care for this interesting case.

Eustachian Tube Shadow – August 1, 2024
A 25-year-old male presents to a rural emergency department after being charged by a cow. The patient has right-sided chest pain, facial bruising lateral to the left eye, and an inability to close his right hand due to pain at the 4th metacarpal. Evaluation of the right ear with the Wispr Digital Otoscope reveals this image.
What is your diagnosis?
Based on the history presented in this vignette, you might expect a diagnosis of hemotympanum (blood behind the eardrum) from a basilar skull fracture. However, this eardrum is normal. In this clinical scenario, the darker area of the eardrum that is circled below might be confused with blood; it is actually the Eustachian tube orifice (tympanic cavity) seen on the other side of the semi-transparent eardrum.

For the eardrum to vibrate properly from sound waves, the pressure on both sides of the eardrum must be the same. This is accomplished by the eustachian tube which connects the middle ear to the posterior nasal cavity. Most of us have had the experience of “popping” our ears when descending in an airplane. This maneuver opens the Eustachian tube and allows the pressure on both sides of the eardrum to equalize. The Eustachian tube can become inflamed and unable to “open.” This causes ear pain from unequal pressure, often confused with acute otitis media.
Here is another case that shows a perforated tympanic membrane where the eustachian tube opening is clearly visible.
The patient, in this case, had a complete trauma workup including CT scans of the head, face, and neck. The only injury found was a fracture at his right 4th metacarpal. An ulnar splint was placed and a follow-up was arranged with orthopedics.
Here is the complete video exam

Chronic Otitis Media with Effusion – July 25, 2024
A 3-year-old child presented to the emergency department (ED) with concern for a fever of 101.3oF at home. His mother reports he had been acting fussy but is otherwise at his baseline of “chronic nasal congestion.” His medical history is significant for speech delay, snoring, and occasional sleep apneic events. He has had a few ear infections in his lifetime, but not recurrent. His last ear infection occurred approximately three months ago and was treated with amoxicillin. During the physical exam, he was found to be well-appearing overall. He has boggy nasal mucosa and 4+ tonsils that are non-erythematous and without exudates. His Wispr digital otoscopic exam is shown.
Which of the following is the most appropriate course of action?
- Treat with high dose amoxicillin
- Treat with acetaminophen
- Referral to an otolaryngologist (ENT) specialist
- Reassurance
Answer: C. Referral to an otolaryngologist (ENT) specialist

The child, in this case, has an amber-colored middle ear effusion (MEE). There is no evidence of infection–no bulging and the malleus landmarks are easily appreciated—thus he may be diagnosed with otitis media with effusion (OME). The amber color is classically observed in MEE that are persistent, thus one could further define his condition as chronic otitis media with effusion (COME). Recurrent acute otitis media (AOM), adenoid hypertrophy, and young age with frequent upper respiratory infections predispose children to COME. This child does not have a particularly high number of AOM diagnoses, but his snoring and occasional sleep apnea episodes suggest upper airway obstruction is likely. Furthermore, the persistence of MEE may impact hearing and result in speech delay, therefore referrals to ENT and Audiology are warranted.
The child was referred to ENT where his audiology exam was remarkable for conductive hearing deficit. He was scheduled to have tonsillectomy and adenoidectomy as well as tympanostomy tube placement the following week.
WiscMed has produced a visual guide to ear conditions that may be found here.
Here is the complete video exam.

Osteoma – July 18, 2024
A 20-year-old female presents to the emergency department (ED) for a headache and sore throat. An incidental physical finding was discovered on her WiscMed Wispr digital otoscope exam. Upon further questioning, the patient denies being a surfer and does not enjoy cold water bathing or swimming.
Regarding the area circled on the image, which feature(s) help determine the most likely diagnosis:
- The lesion is solitary and unilateral
- The patient has never surfed nor had repeated exposure to cold water
- The lesion appears to have a slightly pedunculated base
- Histologic examination of the lesion does not demonstrate layers of new bone
- All the above
Answer: E. All the above

The incidental finding on this patient’s Wispr digital exam is most consistent with a small osteoma in the superior wall of the external auditory canal (EAC). An osteoma is a benign bony neoplasm that can be easily confused with an exostosis, the other common lesion found in the EAC. Osteomas are generally single, unilateral, and have a pedunculated base while exostoses are often multiple, bilateral, and have a wider base.
The two growths can be difficult to distinguish in mild cases by appearance alone. However, they are histologically distinct with exostoses having a laminated appearance representing layers of newly formed bone. This is believed to occur when repeated exposure to cold water triggers periostitis resulting in sequential episodes of osteogenesis, giving rise to the term “surfer’s ear.” Osteomas arise from cancellous bone and lack the layered growth pattern of exostoses. Both lesions are generally asymptomatic unless they enlarge enough to cause conductive hearing loss. In these instances, referral to otolaryngology (ENT) is warranted for further evaluation and potential surgical removal.
Here is the complete video exam
Reference:

Acute Otitis Media with Penicillin Allergy – July 11, 2024
A 6-year-old presents to the emergency department (ED) with fever and ear pain. Her parents report she has had a runny nose and a subjective fever for the past two days. The child began complaining of ear pain earlier in the day but seemed to improve with ibuprofen. However, she awoke that evening with more severe pain and “was burning up,” so she was brought in for evaluation. Her past medical history is significant for recurrent urinary tract infections (UTIs). She has an allergy to Augmentin which has given her hives when taken for UTIs. In the ED, she has a temperature of 39.2o C and is in obvious distress, holding her right ear. Her Wispr digital exam is posted below.
In addition to providing pain control and antipyretic, which of the following is the most appropriate management?
- Amoxicillin
- Ceftriaxone
- Watchful waiting
- Cefdinir
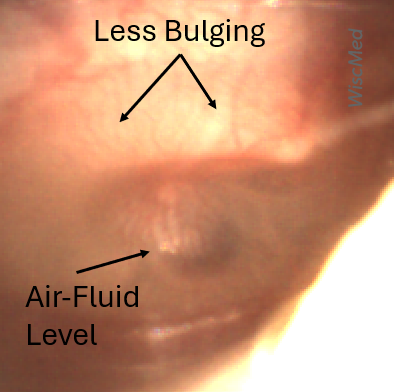
Answer: D. Cefdinir

This child has acute otitis media (AOM) as evidenced by the moderate to severe bulging demonstrated on her Wispr exam. Due to bulging, the bony landmarks of the inner ear are not visible. Given the height of her fever, she can be classified as severe AOM. Accordingly, she should be offered antibiotics for treatment. While high-dose amoxicillin remains the first-line treatment for AOM, alternative therapy is warranted given her history of allergic reaction to amoxicillin. In penicillin-allergic children, cross-reactivity with cephalosporins is significantly lower than the 10% historically reported. In particular, 2nd and 3rd generation cephalosporins have chemical structures that are different enough from penicillin such that the clinically important allergic reaction rate is likely less than 1%. Therefore, both ceftriaxone (intramuscular or IV) and cefdinir would be options for therapy in the child’s scenario. Since this child does not have recurrent AOM, has not been vomiting, and has presumably tolerated oral antibiotics in the past, cefdinir is the most appropriate choice for management.
References to the key action statements from AAP Practice Parameter (Lieberthal et al) in this case:
Clinicians should diagnose acute otitis media (AOM) in children who present with moderate to severe bulging of the tympanic membrane (TM) or new onset of otorrhea not due to acute otitis externa. Evidence Quality: Grade B. Strength: Recommendation.
The management of AOM should include an assessment of pain. If pain is present, the clinician should recommend treatment to reduce pain. Evidence Quality: Grade B. Strength: Strong Recommendation.
Severe AOM: The clinician should prescribe antibiotic therapy for AOM (bilateral or unilateral) in children 6 months and older with severe signs or symptoms (ie, moderate or severe otalgia or otalgia for at least 48 hours or temperature 39°C [102.2°F] or higher). Evidence Quality: Grade B. Strength: Strong Recommendation.
Here is the complete video exam
Additional Reference:

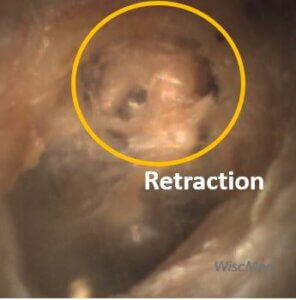
Retraction – June 27, 2024
A 3-year-old female presented to the Pediatric emergency department (ED) with a complaint of congestion and ear pain. Her parents reported the child had multiple upper respiratory infections (URIs) since starting preschool and was treated for ear infections twice. Her most recent ear infection was approximately a month prior to the visit. Earlier in the evening, she was holding her hand over her ear—which her parents interpreted as indicating she was uncomfortable. The child had a runny nose for about a week; however, she has not had a fever. In the ED, she is well-appearing with normal vital signs and mild clear rhinorrhea. Her Wispr digital otoscopic exam is shown.
Which of the following is likely true regarding this child’s presentation?
- Her left tympanic membrane (TM) is retracted
- Her left TM is bulging
- Her right TM is retracted
- Her right TM is bulging
Answer: A. Her left tympanic membrane (TM) is retracted.

This child’s left TM is retracted as evidenced by the prominent lateral process of the malleus in the posterosuperior quadrant. While her retraction is mild, it is easily appreciated when compared to her right TM, which appears normal without the prominent lateral process. Ear laterally can be determined by the orientation of the malleus. Since the malleus is pointing up and to the left, this must be the left ear. Bulging such as from acute otitis media (AOM) is not present.
Retraction of the TM is often a sequela of eustachian tube dysfunction that blocks the normal pressure equalization between the middle and outer ear. As air is reabsorbed by the mucosal lining of the middle ear space, the negative pressure causes the TM to pull inward (i.e., retract) and may result in pain, muffled hearing, or ear popping. Due to children’s horizontally oriented eustachian tubes, frequent URIs, and adenoid hypertrophy, they are particularly prone to eustachian tube dysfunction. Transient TM retractions can be treated with supportive management and brief use of topical anesthetic if there is significant pain. An ENT referral is warranted if the retractions are persistent or worsening. Complications such as hearing loss, retraction pockets (deep localized retractions), progression into perforation, ossicular chain damage, or cholesteatoma may occur.
Here are the complete video exams of both the left and right ear.
Retracted Left TM Video
Normal Right Ear Video

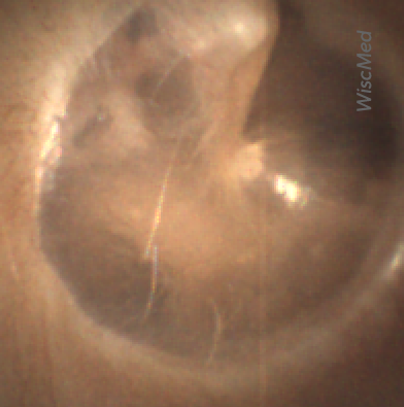
Myringoplasty with Valsalva – June 20, 2024
An exhibitor at the American Academy for Pediatrics (AAP) conference in Toronto stopped by the WiscMed trade show booth. He had heard from other attendees that WiscMed was showing people what their ear drums (Tympanic Membranes, TM) looked like using the WiscMed Wispr digital otoscope. He explains that he had an ear injury that required surgery. The recovery was complicated but at his last visit with otolaryngology (ENT), the physician assured him that his ear was repaired. He’s curious to see what the repair looks like and to know if the repaired TM is intact. The following image of his right ear is obtained.
In this setting, what is the fastest way to determine if the repair is intact?
- Visual inspection
- Tympanometry
- Irrigation
- Valsalva maneuver
Answer: 4. Valsalva maneuver

In the primary care setting, or this case at a trade show, and with a cooperative patient, the Valsalva maneuver is the fastest way to determine if the tympanic membrane (TM) is intact. The Valsalva maneuver is performed by pinching the nostrils closed and applying pressure from the lungs to the mouth area. This is the procedure that is performed when you need to “pop” your ears, for example in a descending airplane. When a Valsalva is performed, the increased pressure in the mouth area is communicated to the middle ear space via the Eustachian tube. The result is that you can clearly see the movement of the ear drum. If the ear drum is not intact (i.e. there is a hole), there will be no movement. Here is the video of the individual performing the Valsalva maneuver. Note the clear outward movement of the TM, indicating that the TM is intact.
Video of exam with Valsalva
Visual inspection alone is not enough to determine if the TM is intact. Even a small defect can cause an air leak. Tympanometry would be the definitive test to interrogate the eardrum. However, it requires a specialized instrument, a tympanometer, that is generally only available in an ENT or audiologists’ office. If there is concern for a TM defect, irrigation would be contraindicated along with being useless for determining the condition of the TM.
Cartilage myringoplasty may be performed for several indications including chronic perforations or conditions causing TM collapse. With its perichondrium intact, cartilage provides a good balance of stiffness to support the TM and elasticity to conduct sound. The surgeon may choose to harvest cartilage from a few sites, including the patient’s own tragus or concha. Once the graft has been attached to the remnant TM, peripheral micro-vessels provide nutrients and help to minimize reabsorption. Hearing often improves with time as the graft continues to soften, enhancing its elasticity and sound conductive properties. The subject of this case reports significant hearing improvement following his surgery and was amazed at the Wispr otoscope being able to visualize the results of his procedure.
Here is the complete video exam without the individual performing the Valsalva.
Video of exam without Valsalva

Epistaxis – June 13, 2024
A 16-year-old male presented evaluation for epistaxis (bloody nose). He states he has had at least five episodes in the past two weeks and mom is concerned he has “lost too much blood.” That evening, the bleeding would not stop despite applying pressure, so he was brought to the pediatric emergency department (ED). He has a heart rate of 75 and is well-appearing without paleness, petechia, or bruising. His WiscMed Wispr anterior rhinoscopic exam is provided below.
Which of the following is true of this patient’s epistaxis?
- The source of the bleeding is likely from the anterior nasal passage
- Dry air may predispose to recurrent episodes
- Bleeding disorders or low platelets are the most common cause
- All of the above
- A and B only
Answer: E. A and B only

This adolescent’s epistaxis is a result of dilated blood vessels located on the anterior inferior nasal septum (see Wispr image). As the most common site of epistaxis in children, this area of the septum is also known as Little’s Area or Kiesselbach’s plexus.
Epistaxis is a common pediatric complaint with approximately 250,000 visits annually in the U.S. The mean age is 8 years old and more than 50% of children over 5 years have had at least one episode. Most cases can be traced to dilated vasculature in Kiesselbach’s plexus which are often visible on physical exam. The overlying nasal mucosa is quite thin and susceptible to irritation from dry air, irritants, and digital trauma (i.e. nose picking), leading to episodes that, while occasionally frequent, rarely lead to anemia or life-threatening blood loss in an otherwise healthy child. Indications for additional evaluation include the very young child (epistaxis is rare in children less than 2 years) or if there is a history of excessive bleeding (ex. with circumcision or menarche), paleness, petechia, or bruising.
Management of the anterior nosebleed is dependent on the number and severity of episodes as well as the presence of visibly dilated vessels. Stopping the bleeding is typically accomplished with direct pressure (no “peaking” for at least 20 minutes) augmented with Oxymetazoline (Afrin, or similar vasoconstrictor) soaked cotton ball. Once bleeding is controlled, direct visualization of the offending vessels may be accomplished with a good light source, aided by anterior rhinoscopy. When episodes are recurrent, and the dilated vessels are apparent, chemical cautery with silver nitrate is a quick and effective procedure to reduce recurrence (see referenced link for a video of the procedure). This intervention was elected by the patient with satisfactory results (see image 2). He was discharged with recommendations to protect the mucosa with a non-irritating emollient such as Vaseline as well as ENT follow-up if rebleeding occurs.
References:
Tabassom A, Dahlstrom JJ. Epistaxis. [Updated 2022 Sep 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK435997/
https://www.youtube.com/watch?v=F1v4wtf-i2U
Here are the complete video exams
Initial Examination Video
Post Cauterization Video

Perforation – June 6, 2024
A 16-month-old presents to the emergency department (ED) with congestion and fever for one day. Her mom is worried she may have an ear infection due to past ear complaints, including a procedure performed on her left ear 5 months ago. Mom reports this surgery was necessary after her daughter had ear drainage and a diagnosis of ruptured left eardrum when she was only 4 weeks old. The child recovered uneventfully, and the current complaint is her first febrile illness since the surgery. In the ED, she is well-appearing and has mild upper respiratory (URI) symptoms. Her Wispr digital otoscopic exam is shown.
Which of the following does her Wispr exam demonstrate?
- Cholesteatoma
- Tympanic perforation
- Myringosclerosis
- Acute otitis media (AOM)
- B & C
Answer: E. Both tympanic perforation and myringosclerosis.

The child’s Wispr exam demonstrates both myringosclerosis (anterior superior) and a tympanic membrane (TM) perforation (posterior inferior). There is no drainage or bulging to indicate acute otitis media (AOM). Upon further review of the child’s medical records, the procedure performed on her left TM was a resection of a congenital cholesteatoma and gelfoam tympanoplasty. The gelfoam has been extruded/absorbed and she has a resultant perforation that is closely monitored.
A cholesteatoma is an epithelial-lined cyst of the TM that may invade the middle ear space and impact hearing. Congenital cholesteatomas appear as small pearly bumps, typically on the anterior portion of the TM (image). While felt to be relatively rare, the incidence of congenital cholesteatomas is likely underestimated with one review estimating as high as 24%. In the current case, the unusual drainage and concern for AOM in the neonatal period led to an appropriate referral to the Pediatric ENT specialist.
On this visit, no action is required.
Here is the complete video of the exam.
Reference:

Bilateral AOM – May 30, 2024
A six-month-old male is brought into the pediatrician’s office with concern for fever and fussiness. The child has been generally healthy and is fully immunized. The mother reports that the day-care attending child developed a cough and runny nose 3 days ago. Yesterday, he developed a fever of 101.5 F. The mother has been pushing fluids and providing acetaminophen. On physical exam, the child appears ill without being toxic. He appropriately resists the exam. His mucous membranes are moist, and his capillary refill is less than a second. His temperature is 102 F. The following image of his left tympanic membrane (TM, “ear drum”) is obtained with the WiscMed Wispr digital otoscope.
What is the next step in management?
- The child should be admitted to the hospital for fluids and IV antibiotics.
- The child should be discharged on oral antibiotics with careful return instructions.
- The mother should be reassured and continue her home treatment.
- An urgent consultation with otolaryngology (ENT) for ventilation (ear tubes) should be placed.
Answer 2. The child should be placed on oral antibiotics with careful return instructions.

The child has acute otitis media (AOM). The eardrum is severely bulging, there is erythema (redness) and loss of bony landmarks. This would be classified as severe AOM. In fact, the child has AOM in both ears. Compare these images of AOM with a normal ear.
American Academy of Pediatrics (AAP) treatment guidelines are for initiating antibiotics for severe AOM. Since the child is well-hydrated and non-toxic, there is no indication for hospital admission. The child does not have a history of ear infections, so ear tubes are not indicated now.
WiscMed has created a visual diagnosis of ear conditions, which may be found here.
Here are both the left and right ear videos.
Left Ear AOM Video
Right Ear AOM Video

Myringoplasty – May 23, 2024
The following Wispr digital otoscope video and image are obtained from a 43-year-old male attending a medical conference. He reports having complicated auditory issues and, as a young adult, underwent a procedure to help improve his hearing. While he continues to require hearing assistance, he reports the procedure was successful.
True or False
This subject has extensive myringosclerosis which is likely the etiology of his hearing deficits.
Answer: False

The Wispr image and video demonstrates extensive shiny, white “lumps” obscuring all bony landmarks of the subject’s tympanic membrane (TM). One gets the sense these are located just deep to the outer layer of his TM. While myringosclerosis can also be very extensive, it typically appears as white scarred areas on the superficial epithelium of the TM and does not impressively obscure the normal bony landmarks. A review of the images with an ENT specialist confirmed the subject of this case had a cartilage myringoplasty as part of the management of his complex hearing problems.
Cartilage myringoplasty may be performed for several indications including chronic perforations or conditions causing TM collapse. With its perichondrium intact, cartilage provides a good balance of stiffness to support the TM and elasticity to conduct sound. The surgeon may choose to harvest cartilage from a number of sites, including the patient’s own tragus or concha. Once the graft has been attached to the remnant TM, peripheral micro-vessels provide nutrients and help to minimize reabsorption. Hearing often improves with time as the graft continues to soften, enhancing its elasticity and sound conductive properties. The subject of this case reports significant hearing improvement following his surgery and was amazed at the Wispr otoscope being able to visualize the results of his procedure.
Here is the complete video exam.
Nasal Septal Hematoma – May 16, 2024
A 30-month-old presents to the emergency department (ED) for evaluation of a nosebleed (epistaxis). Mom reports the child had an injury two nights ago when he jumped off his bed and struck his face on the nightstand. The child was taken to a local ED where he was noted to have a bloody nose and a small laceration to the base of his nose. The laceration was repaired with three sutures and the child was discharged. His mother reports that the child has continued to have bleeding from the right nostril and seems congested. His physical exam is notable for extensive bruising to the tip of the nose and below both eyes. There are two sutures in place to the right lower ala with a small amount of bleeding at the site. His interior nasal exam, utilizing the Wispr digital otoscope for anterior rhinoscopy, is shown.
Which of the following is indicated based on the child’s findings?
- Emergency physician consultation with otolaryngology (ENT) for urgent management
- Referral to ENT for management in the outpatient setting
- Cautery of the lesion with silver nitrate
- Oxymetazoline (Afrin) spray and nasal packing in ED, follow-up with the primary physician
Answer: A. Emergency physician consultation with otolaryngology (ENT) for urgent management

The child’s Wispr exam demonstrates a right-sided nasal septal hematoma. The hematoma is seen as a bluish bulge on the upper nasal septum and is contributing to the ongoing epistaxis and “congestion” noted by his mother. Nasal septal hematomas require immediate evacuation to relieve pressure necrosis of the septal cartilage which can result in complications including septal perforation, abscess, or collapse of the nose (“saddle deformity”). Otolaryngology (ENT) was consulted, and a maxillofacial computed tomography (CT) was recommended. The CT demonstrated a non-displaced nasal fracture and confirmed the septal hematoma. The patient was taken to the operating room where the hematoma was drained and splinted. Upon follow-up, he was doing well, and the family expressed gratitude for his expedited care.
Here is the complete video of the nasal exam. Note the usefulness of the Wispr’s video capability in this squirming child.

Osteoma – May 9, 2024
A healthy 48-year-old man from Finland visited the WiscMed booth at the Pediatric Academic Society conference in Toronto. He has no ear or hearing concerns (other than spousal selective hearing).
The following image of his ear drum was obtained with the WiscMed Wispr digital otoscope.
Which of the following is true?
- The patient has a history of ear infections.
- The patient has had consistent exposure to cold water.
- The ear is normal.
- The patient has a benign finding that does not require further action.
Answer D. The patient has a benign finding that does not require further action.

The patient has two benign findings that require no action. First is an osteoma. This is a benign growth of bone in the external ear canal. It often appears pedunculated. It has no clinical significance unless it is large enough to interfere with hearing or cause external otitis. Second is a pseudo retraction of the pars flaccida portion of the tympanic membrane (TM). The TM normally “drapes” over the anterior-superior portion of the drum. In this case, the TM is retracted, likely an anatomic finding associated with a slightly more horizontal malleus.
Consistent exposure to cold water such as a surfer may experience often causes exostosis. This is also a benign growth of the bone in the external ear canal. Exostosis is generally further from the ear drum and has a broader base than an osteoma.
There is no sclerosis as would be found in someone with a history of ear infections and ear tubes.
Here is the complete video exam.
Reference
Carbone PN, Nelson BL. External auditory osteoma. Head Neck Pathol. 2012 Jun;6(2):244-6. doi: 10.1007/s12105-011-0314-7. Epub 2011 Dec 20. PMID: 22183765; PMCID: PMC3370017.

Periosteal Abscess – May 2, 2024
A 5-year-old female with mild autism is referred to the emergency department (ED) from Urgent Care (UC) for evaluation of an enlarged lymph node behind the right ear. The mother states the child does not complain of pain very often “even when sick.” She was concerned when her daughter had a fever of 103oF at home. At the UC, she was noted to have a tender lymph node which raised concern for an abscess. In the ED, the child was afebrile and generally well-appearing. Her HEENT exam was notable for her right external ear appearing quite prominent and a 3×3 cm semi-fluctuant posterior auricular mass with overlying skin erythema. Her left ear appeared normally positioned but with a smaller 1X1cm mass behind the external ear. Pulling externally on her ears did not elicit pain. Her right ear Wispr digital otoscope exam is shown.
Which of the following is true regarding the child’s presentation:
- She has acute otitis media (AOM) and should be treated with oral antibiotics and close follow-up.
- She has external otitis media (EOM) and should be treated with topical antibiotics and close follow-up.
- Imaging with contrast computed tomography (CT) is indicated.
- An ultrasound (US) of the posterior auricular mass with aspiration of any fluid for culture is indicated.
Answer: C. Imaging with contrast computed tomography (CT) is indicated.
The differential diagnosis of pediatric posterior auricular masses includes lymph node pathology, abscess, various cysts, hematoma, and occasionally malignancies. An ultrasound (US) is often helpful, and aspiration or incision and drainage may be necessary. However, in a child with fever, ear malposition, and posterior auricular swelling, cross-sectional imaging (CT) to evaluate for complications of mastoiditis such as subperiosteal abscess is indicated. The pathophysiology and complications of mastoiditis have previously been discussed here. Although the right external auditory canal does not appear normal, there is no significant swelling nor is there pain with manipulation of the external ear that would indicate external otitis media (EOM).

Looking carefully at the image, or the video (below), besides the obvious canal “blister,” the child also has acute otitis media (AOM) in the right ear. However, given the presence of the ear canal anomaly, concern is heightened for pathology more serious than simple AOM. The child had a contrast CT performed which demonstrated bilateral mastoiditis with subperiosteal abscesses. The blister-like appearing mass in the right external ear canal (EAC) was unroofed during surgery and noted to have serous fluid. The surgeon felt this was likely reactive from the nearby abscess.
Here is the complete video exam

Resistant Acute Otitis Media – April 25, 2024
A three-year-old male presents to the emergency department (ED) for “medication management” after a recent diagnosis of acute otitis media (AOM). His family reports the child has had multiple bouts of AOM with his most recent diagnosis three days ago. Two weeks prior, he was treated for his fourth AOM in five months. He completed a course of antibiotics without difficulty, however, he continued to stick his finger in his ears and seemed uncomfortable. The parents had their child re-evaluated and bilateral AOM was noted. A discussion of prior management revealed he had been treated with four different antibiotics. He has an appointment with ENT in three months, the earliest he could get in. At the time of his current diagnosis, a plan for three days of intramuscular (IM) antibiotics was agreed upon. He received his first two doses without difficulty and presented to the ED for his third dose due to the schedule falling on a weekend. Of note, the family was turned away from an Urgent Care who refused to administer “too much” ceftriaxone. His Wispr digital otoscope exam from his current visit is shown.
Which of the following is correct regarding this child’s presentation?
- His initial diagnosis of AOM is incorrect and he does not require an intramuscular antibiotic.
- His initial diagnosis of AOM is correct but he should be treated with an oral antibiotic.
- His current exam demonstrates persistent AOM and referral for immediate tympanostomy (ear tubes) is indicated.
- His current exam indicates improvement and continued treatment with 3rd dose of intramuscular antibiotic is appropriate.
Answer: D. His current exam indicates improvement and continued treatment with 3rd dose of intramuscular antibiotic is appropriate.
The child’s initial Wispr exam demonstrates AOM as evidenced by severe bulging. His repeat exam following the two doses of IM antibiotics demonstrates improvement with significantly less bulging.
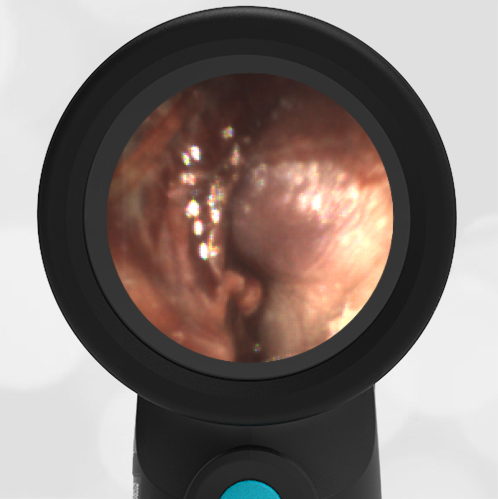
He continues to have a cloudy middle ear effusion (MEE), but this would be expected only two days into treatment. The air-fluid level suggests that the Eustachian tube is now venting the middle ear space. Given the improvement, there is no current indication for ear tubes. While single dose IM ceftriaxone is an acceptable option for children who do not tolerate oral medications, it may not be sufficient in children with multiple treatment failures. Therefore, given his history of difficult-to-clear AOM, continued treatment with the third dose of IM antibiotics is appropriate.
While treatment strategies will continue to evolve, the following diagram from aafp.org utilizes the 2013 AOM Practice Parameter:
References:
Leibovitz E, Piglansky L, Raiz S, Press J,Leiberman A, Dagan R. Bacteriologic and clinical efficacy of one day vs. three-day intramuscular ceftriaxone for treatment of nonresponsive acute otitis media in children. Pediatr Infect Dis J. 2000;19(11):1040–1045.
Lieberthal AS, Carroll AE, Chonmaitree T, Ganiats TG, Hoberman A, Jackson MA, Joffe MD, Miller DT, Rosenfeld RM, Sevilla XD, Schwartz RH, Thomas PA, Tunkel DE. The diagnosis and management of acute otitis media. Pediatrics. 2013 Mar;131(3):e964-99. doi: 10.1542/peds.2012-3488. Epub 2013 Feb 25. Erratum in: Pediatrics. 2014 Feb;133(2):346. Dosage error in article text. PMID: 23439909.
Here is the complete video exam

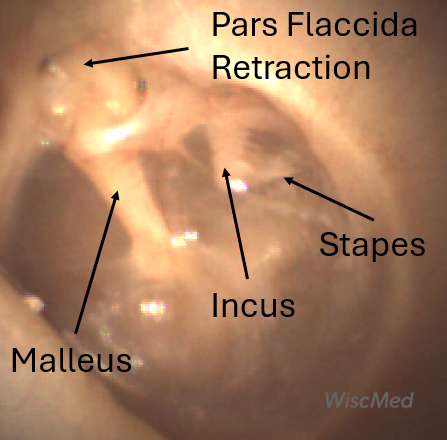
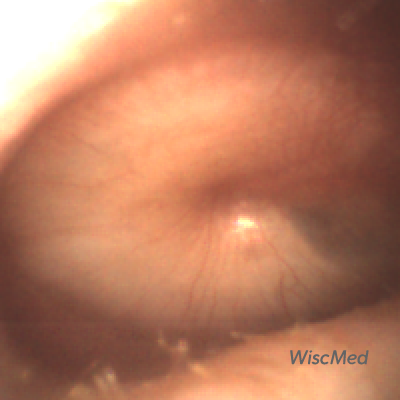
Pars Flaccida Retraction – April 18, 2024
An attendee at the Urgent Care Conference visited the WiscMed tradeshow booth. The following image of her left ear was obtained with the WiscMed Wispr digital otoscope.
Which of the following is true?
- She’s had an eardrum perforation in the past.
- Her ear is normal.
- She should be referred urgently to an otolaryngologist (ENT).
- The pars flaccida portion of her tympanic membrane (TM, “eardrum”) is retracted.
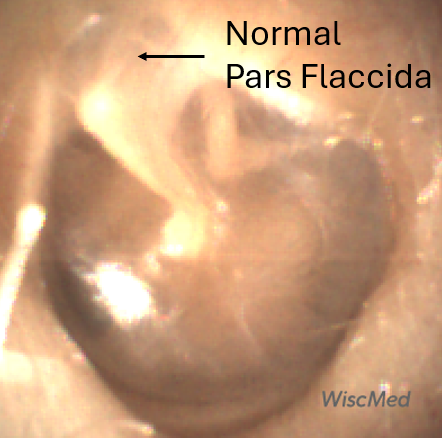
Answer: 4. The pars flaccida portion of her tympanic membrane (TM, “ear drum”) is retracted.
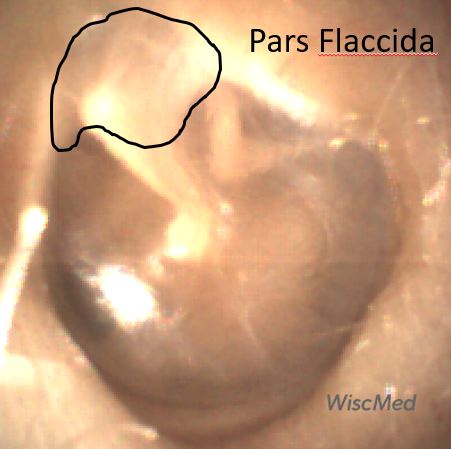
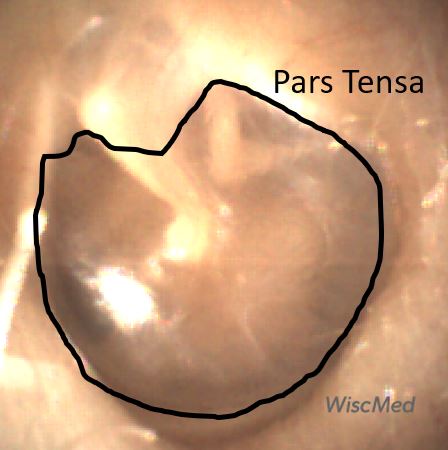
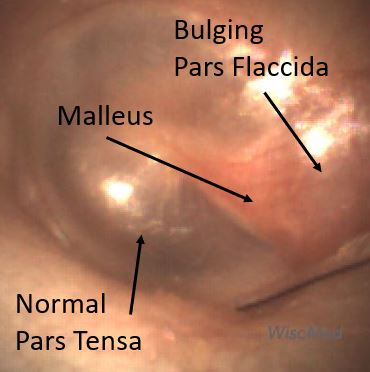
The attendee has a retraction of the pars flaccida portion of her eardrum. The eardrum consists of two regions, the pars flaccida and the pars tensa.
The pars tensa is the portion of the tympanic membrane that is the largest. It’s what people tend to think of when they think of the “eardrum.” As the name suggests, it is “taut,” much like if you stretched plastic wrap on top of a bowl. You could also imagine the pars tensa to be similar to a drum surface. It is the portion of the eardrum responsible for translating sound waves into mechanical movement.
The pars flaccida, as the name suggests, is less “taut” and also thicker. It drapes across the superior portion of the malleus. Although it does not have an active role in sound wave transcription, it is necessary to provide complete coverage of the middle ear space and allow for the proper functioning of the pars tensa.
From a clinical perspective, the pars tensa gets most of our attention. This is the place where we would expect to see perforations, effusions, and the characteristic bulging of acute otitis media.
The pars flaccida may be the first place that bulging of the tympanic membrane is seen due to increased pressure in the middle ear space. The pars flaccida is where most eardrum movement would be appreciated if evaluating mobility of the eardrum via either pneumatic otoscopy or a Valsalva maneuver.
A pars flaccida retraction is of little clinical significance. If severe, it could limit mobility of the incudomalleolar joint and cause hearing loss. There is no indication that the attendee has had an eardrum perforation. There is no indication for a referral to otolaryngology.
Here is the complete video exam

Acute Otitis Media – April 11, 2024
A 3-year-old female presents to the emergency department (ED) with ear pain and a temperature of 102o F. Her mother reports her daughter initially complained of left ear pain last night, but this morning seemed to be holding her right ear. Her Wispr digital otoscope exam is shown.
Which of the following is true?
- The child has acute otitis media (AOM).
- The child should be initiated on a 7-day course of antibiotics.
- The image is of the child’s right tympanic membrane (TM).
- A & B
- All of the above
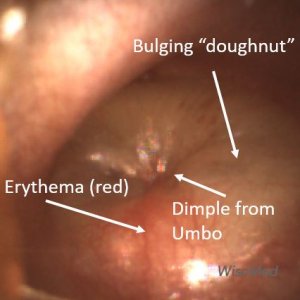
Answer: E
The child’s Wispr exam demonstrates moderate to severe bulging, evidenced by the donut appearance of the tympanic membrane (TM, “eardrum”). Given her symptoms of pain and fever, she should be started on antibiotics. The symptoms and physical exam are diagnostic of acute otitis media (AOM), an infection in the middle-ear space. Since she is older than two years of age, seven days is an appropriate duration of treatment. WiscMed has created a guide to AOM treatment that can be found here.
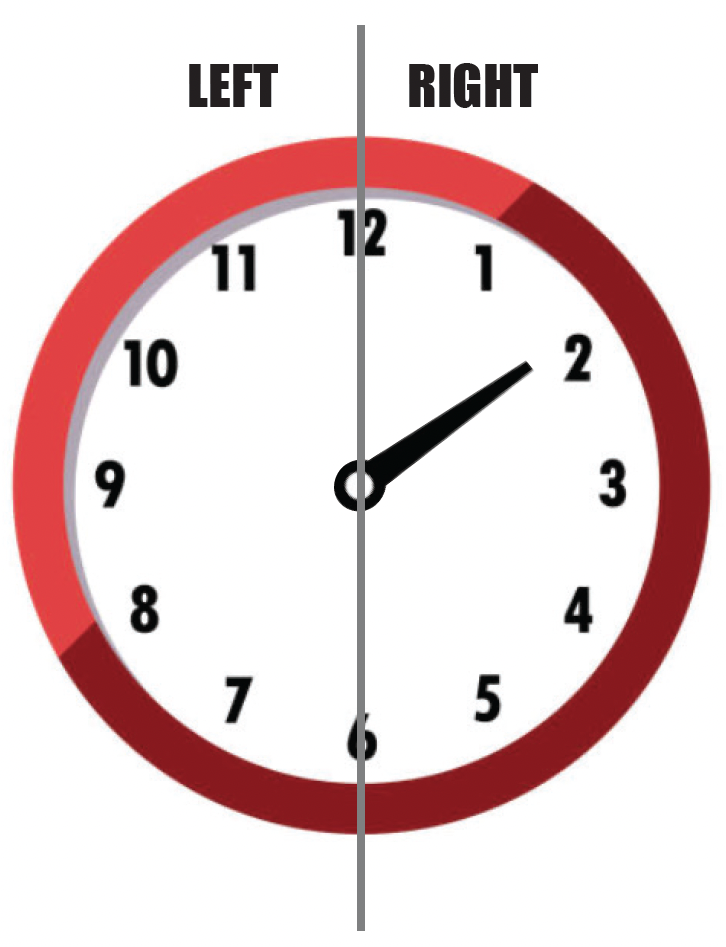
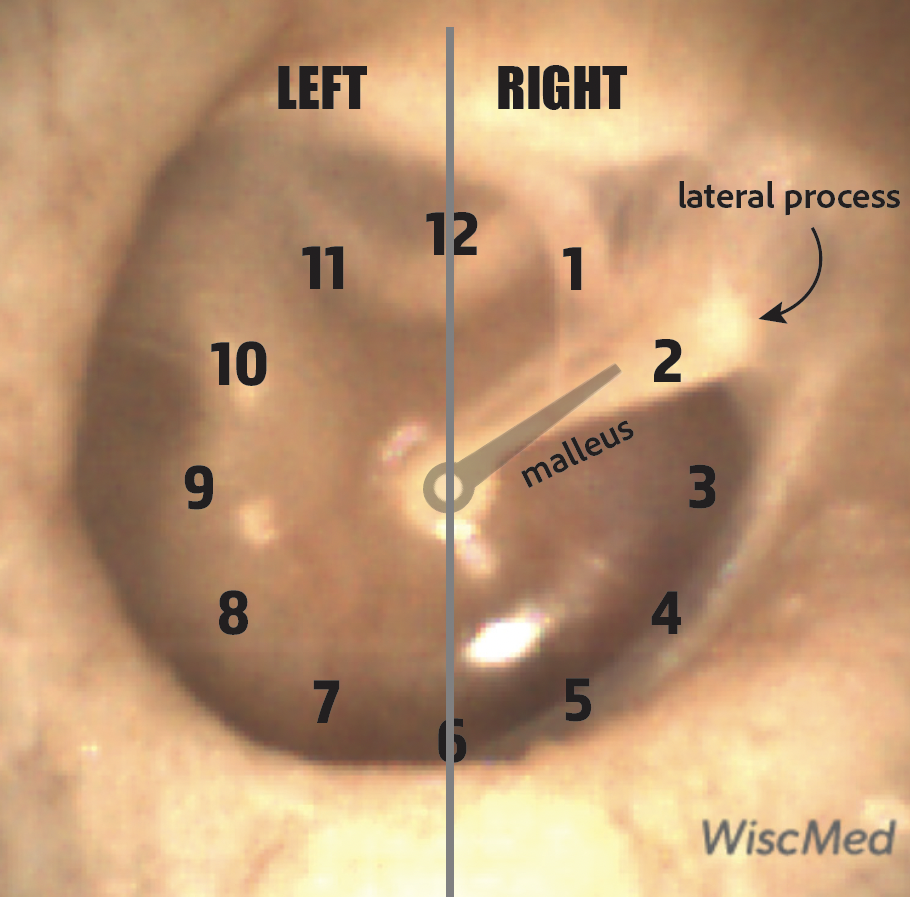
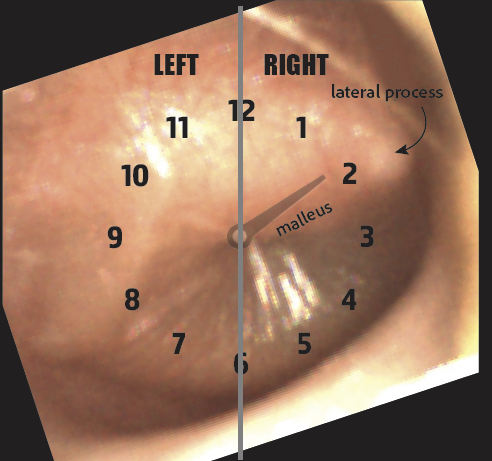
Determining the laterality of the TM is simpler when there is no bulging since the bony malleus orientation provides the necessary clue. Imagining the TM as a clock, the malleus represents one of the hands. If the hand points to the right side of the clock (roughly toward 2 o’clock), then it is the right TM. Conversely, if the hand points to the left side of the clock (roughly toward 10 o’clock) it is the left TM. Here is an illustration of this concept on a healthy and normal right TM.
With bulging from AOM, the bony landmarks become less obvious, and identifying laterality is more challenging. However, with knowledge of the normal malleus position, look for the tip of the lateral process as a small white “point” along the periphery. Recognition of these relationships makes the process simple. Thus the TM in question is from the child’s right ear. Note that if the bulging from AOM is severe, no portion of the malleus will be visible and determination of the laterality may be impossible from inspection alone.
Here is the complete video exam

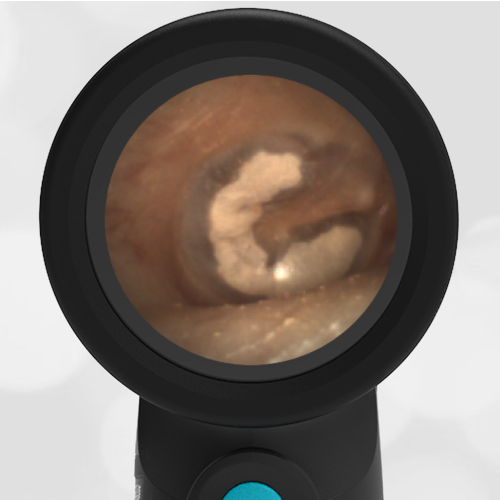
Myringosclerosis and Myringoplasty – April 4, 2024
A 6-year-old presented to an Urgent Care (UC) with fever for 5 days. His mother reports he has had an upper respiratory infection for the past week and recently tested negative for influenza. This morning he felt warm, complained of headache, and had an increased nasal discharge. His parents called the nurse triage line and were directed to the UC where his temperature was 103.7oF. His Wispr digital exam is shown below. Aside from copious nasal discharge, the remainder of his physical exam was unremarkable.
Which of the following is true regarding this child’s presentation?
- He has acute otitis media (AOM) and antibiotics should be considered.
- He has a history of ear infections.
- He likely suffers from conductive hearing loss.
- He has a middle ear effusion.
Answer: B. He has a history of ear infections.
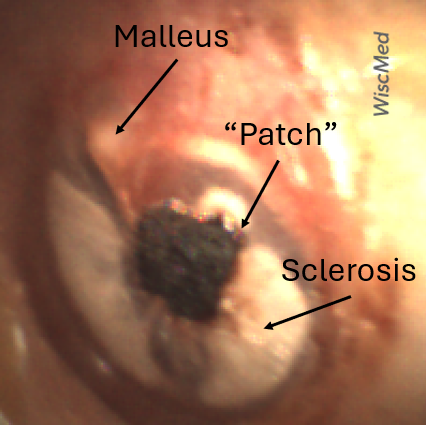
While the child’s clinical scenario of persistent fever, headache, and green nasal discharge is suggestive of sinusitis requiring antibiotics, his ear findings do not support the diagnosis of acute otitis media (AOM). However, the child’s Wispr exam does demonstrate impressive myringosclerosis characterized by the white plaques along the periphery of both tympanic membranes (TM). Myringosclerosis is a condition of calcification and hyalinization of the TM that may occur in the setting of chronic inflammation from recurrent ear infections, trauma, or following tympanostomy tube (TT) placement. Despite its appearance, myringosclerosis does not typically result in hearing loss. There is no fluid behind the TM which would be the hallmark of a middle ear effusion.
The child also has dark clotted-appearing areas, “patches,” that are not consistent with myringosclerosis. Further questioning of the parents elicited a past medical history that included frequent ear infections as a younger child. He had TTs placed four years ago which were noted to still be present at his most recent health maintenance visit. TTs typically fall out within 18 months and may cause chronic perforation if they have not spontaneously extruded by three years. For this reason, the child had the tubes removed one month prior. The darkened areas are the Gelfoam myringoplasties that were also performed to patch the resulting defects and promote healing.
Here is the complete video exam.
Recent Acute Otitis Media – March 28, 2024
A 3-year-old presents to the emergency department (ED) for congestion, cough, and shortness of breath. Her parents report this is her second or third “cold” since starting daycare two months ago. The child is afebrile and generally well-appearing. She has mild wheezing on auscultation that resolves with albuterol. Her Wispr digital otoscope exam is shown.
Which of the following can be inferred from the tympanic membrane (TM) findings?
- She recently had acute otitis media (AOM).
- She has had multiple ear infections and tympanostomy tubes (TT).
- She previously had a ruptured tympanic membrane (TM, “ear drum”).
- Given her history, an urgent, but not emergent consult to otolaryngology (ENT) is indicated.
Answer: A. She recently had acute otitis media (AOM).
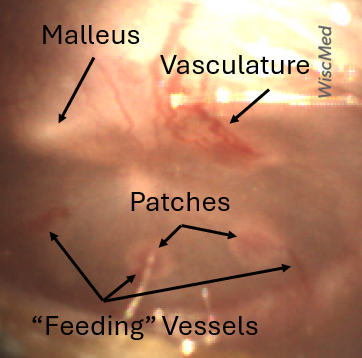
The child’s Wispr exam demonstrates several small circular patches along the periphery of the tympanic membrane (TM, “ear drum”). These patches of mucopurulent material are on the “inside” of the TM and may appear during the recovery phase of acute otitis media. In the image, small blood vessels involved in healing are also easily appreciated. Dr. Michael Poole in his book, “Otitis, the Expert’s Diagnostic Guide” refers to these small blood vessels as sentinel vessels or feeding vessels (chapter 9.2). Tympanosclerosis (also termed myringosclerosis) are areas of thickened TM resulting from recurrent AOM, injury, or tympanostomy tubes. Tympanosclerosis is not present here. AOM recovery patches are transitory, while tympanosclerosis is permanent and appears as asymmetric white plaques that lack vasculature. There is no indication of a past perforation. There is no indication for a referral to ENT.
Here is the complete video exam
Acute Otitis Media – March 21, 2024
A 5-year-old male presents to the emergency department (ED) late in the evening with ear pain. His mother reports her son first reported ear discomfort two days prior, but he seemed fine after a dose of ibuprofen. She did not seek evaluation. This evening, he woke up crying and holding his right ear. When asked how much his ear hurts, he replies “really, really bad”. In the ED, he is afebrile and has normal age-appropriate vital signs. Aside from being tearful, he appears well without any other significant findings. His Wispr digital otoscope exam is shown.
Which of the following is/are true regarding this child’s presentation?
- The child does not have acute otitis media (AOM).
- His symptoms are severe, so management should include pain control and starting antibiotics immediately.
- His symptoms are mild, so management should include pain control and observation with follow-up if his symptoms persist beyond the next 48-72 hours.
- An urgent consult to otolaryngology (ENT) is indicated for consideration of ventilation (ear) tubes.
Answer: B
Management of children for acute otitis media is a three-step process: making the diagnosis, assessing severity, and determining the treatment.
1. Making the Diagnosis
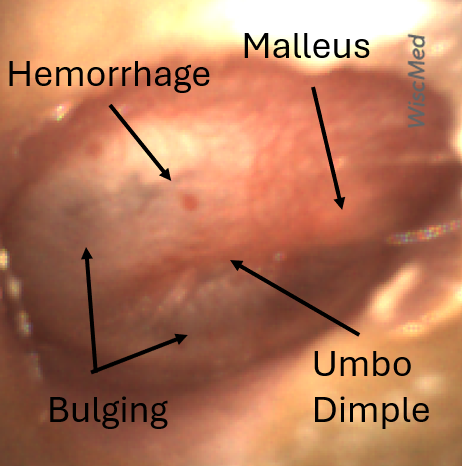
The child’s Wispr exam demonstrates mild bulging and erythema (and a few small areas of hemorrhage) of the left tympanic membrane (TM). According to the AAP Practice Parameter, “clinicians should diagnose AOM in children who present with mild bulging of the TM and recent (less than 48 hours) onset of ear pain (holding, tugging, rubbing of the ear in a nonverbal child) or intense erythema of the TM.”
While moderate to severe bulging is readily apparent as the TM demonstrates the “donut sign”, mild bulging is less obvious. However, a closer look at the TM allows one to discern findings that give the TM a “full” appearance in mild bulging: a dimple centrally (where the umbo is a fixed attachment) and difficulty visualizing the malleus superiorly (where the pars flaccida is the first portion of the TM to bulge outward).
Thus, the child has acute otitis media (AOM).
2. Assessing Severity
Severity is determined by the duration of symptoms, degree of pain, and height of fever. According to the AAP Practice Parameter, severe signs or symptoms include moderate or severe otalgia, otalgia for at least 48 hours, or temperature 39°C or higher. In the current case, his symptoms were assessed as being severe given that ear discomfort started two days prior and seemed to be worsening.
3. Determining Treatment
Treatment always includes the management of pain, so oral and topical analgesics should be recommended. Initiating antibiotics depends on the severity, uni- versus bilateral involvement, and age. The AAP recommends treating all severe AOM immediately, regardless of age or laterality, thus immediate initiation of antibiotics would be most appropriate in the current case.
Since the child has no history of recurrent AOM, there is no indication for referral to ENT for ventilation tubes.
WiscMed has created a visual guide to ear conditions that can be found here. In addition, here is a guide to AAP recommendations for AOM.
Here is the complete video exam.
Reference:
Lieberthal, et al. The Diagnosis and Management of Acute Otitis Media. Pediatrics (2013) 131 (3): e964–e999.

Bilateral Acute Otitis Media – March 14, 2024
A 4-year-old female is brought into the emergency department (ED) at 2 am for ear pain. The parents say that the child has had a cough, low-grade fever, and a runny nose for the past 3 days. Yesterday, she began to complain of pain in both ears and says the left ear hurts worse than the right ear. The parents gave the child Tylenol, which was only partially helpful in controlling the pain. The child has been unable to sleep. The child has had several episodes of ear infections in the past. The following image of her left ear is obtained with the WiscMed Wispr digital otoscope.
What is the next step in management?
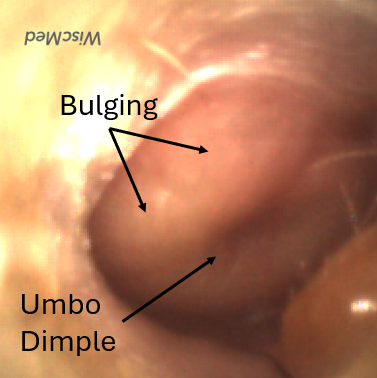
The child has acute otitis media (AOM) in her left ear.
Based on the American Academy of Pediatrics (AAP) guidelines, this would be considered a severe case of AOM. The features that make this case severe include severe bulging, increased pain, and increased erythema (redness). Note that there is complete loss of visualization of the bones of the middle ear due to the bulging. The umbo dimple (caused by the attachment of the distal malleus to the eardrum) is pronounced.
It’s interesting to compare the child’s left ear to her right ear.
Note that the right ear also has bulging. However, the bulging is not as marked as in the left ear. The lateral process of the malleus is still discernable. In addition, the umbo dimple is not as pronounced. This would be considered moderate bulging. The moderate bulging with ear pain would still classify this ear as being severe AOM.
Given that the child has severe AOM in both ears and that she is 4 years old, the AAP guidelines recommend 7 days of antibiotics.
The AAP AOM practice guidelines can be found here. In addition, WiscMed has created a visual guide to common ear conditions that can be found here.

Foreign Body – March 7, 2024
A healthy 18 year-old-female presents to the allergy clinic for evaluation. She has no history of ear problems, nor does she have any ear complaints. As part of the complete physical examination, the following image of the patient’s left ear is obtained with the Wispr digital otoscope.
What is the next step in management?
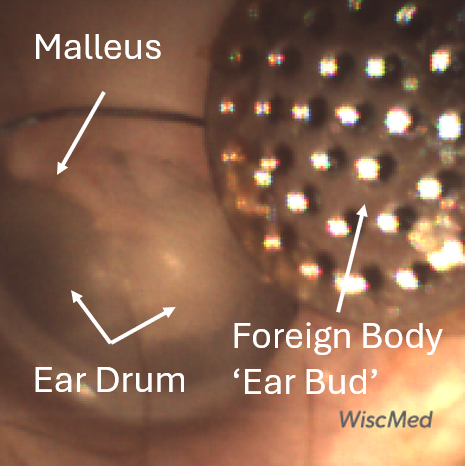
The patient has an incidental finding of a foreign body in the external ear canal. This should be removed. It’s surprisingly common for people to have foreign bodies in their ear canals and not be aware. Here is another case that demonstrates a similar scenario. The image clearly shows the foreign body lodged some distance away from the tympanic membrane (TM, ear drum). In addition, the TM appears healthy with no erythema or perforation. The malleus is clearly visible. In a cooperative adult, there are several choices for foreign body removal. Techniques could include forceps, lavage, or Katz extractor. In this case, the foreign body was uneventfully removed with lavage. Here is a photo of the foreign body after removal. The patient recognized the item as part of an earbud.
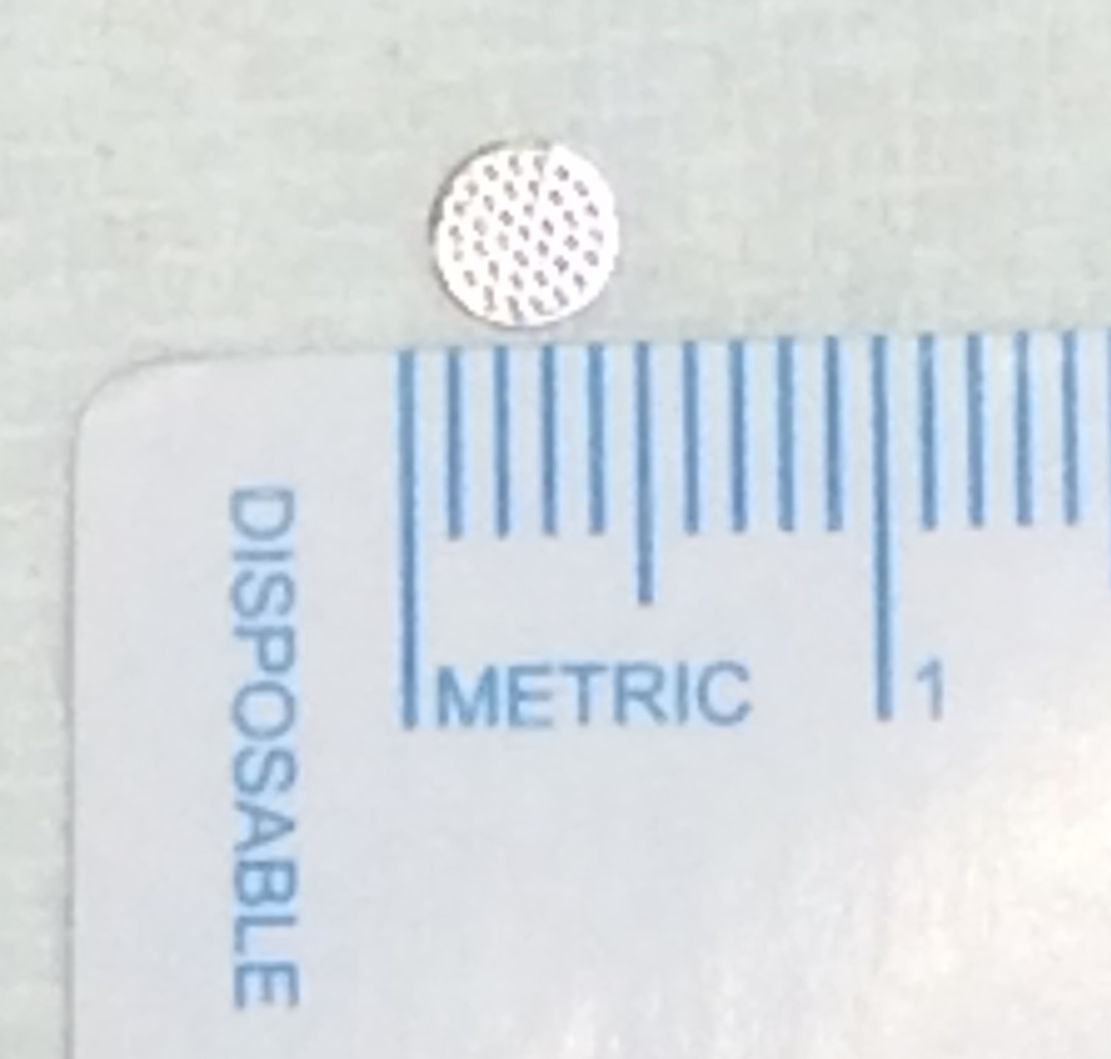
WiscMed thanks James Thompson, MD of Chisholm Trail Allergy and Asthma in Fort Worth, TX for this week’s interesting case.

Otitis Media with Effusion – February 29, 2024
A 9-month-old female presents to the emergency department (ED) with her parents with concern for “many ear infections” and to obtain a second opinion. The parents state the child has been on antibiotics three times in the past four months and was prescribed another antibiotic earlier in the day when she was evaluated in Urgent Care. They report the child has an upper respiratory infection, but no fever. Her last ear infection was two weeks earlier and she was treated with a “white antibiotic.” In Urgent Care, her parents felt the ear exam was a struggle and wanted to be sure another course of antibiotics was necessary. They also report their daughter has a diaper rash and struggles with GI issues. In the ED, the child is afebrile and well-appearing. She has mild nasal congestion but clear lung sounds and no increased work of breathing. She has a beefy red rash in her diaper area.
Her Wispr digital otoscope exam is shown.
What is the appropriate course of action:
- Reinforce the need for taking the oral antibiotic prescribed in the Urgent Care.
- Stop the oral antibiotic and recommend an intramuscular antibiotic instead.
- Stop the antibiotic and treat her diaper rash with topical antifungal.
- Recommend immediate referral to ENT for tympanostomy tube placement.
Answer: C. Stop the antibiotic and treat her diaper rash with topical antifungal.
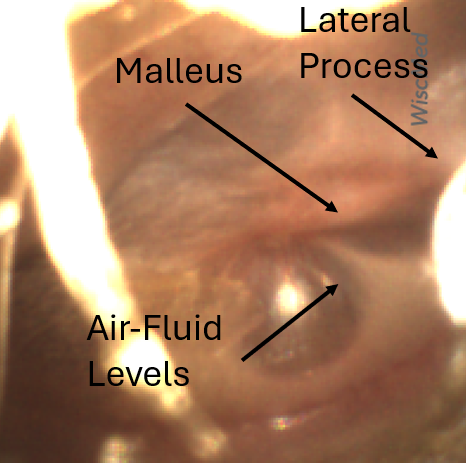
This child has a somewhat cloudy middle ear effusion (MEE) as evidenced by multiple air-fluid levels visualized on her Wispr exam. Air-fluid levels generally indicate that the middle ear space is being ventilated by the Eustachian tube. While the lateral process is slightly obscured, one can easily make out the length of the malleus and there is no “donut sign” to indicate moderate to severe bulging. Furthermore, the tympanic membrane (TM, “ear drum”) is nicely translucent without intense erythema. Thus, this child does not have acute otitis media (AOM) and her diagnosis is most consistent with otitis media with effusion (OME). She does not require antibiotics but ought to have her diaper-area candidiasis treated with a topical antifungal. Tympanostomy (“ventilation, ear”) tubes are indicated with recurrent AOM.
This case was notable for the challenging exam encountered in Urgent Care. Note the initial view below. This would be all a traditional otoscope would have seen given the wax burden. The Wispr digital otoscope is able to navigate around the wax to give a diagnostic view. See the complete video at the end of this case to appreciate this navigation.
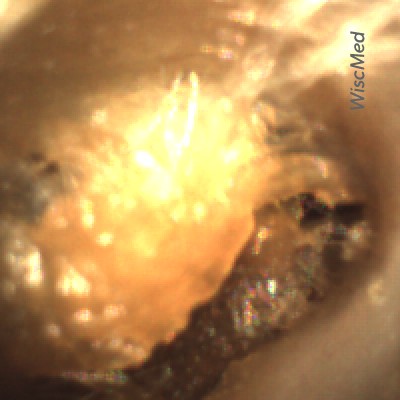
Cerumen (wax) burden in the external ear canal
A partial and fleeting view of the TM could easily be misdiagnosed as AOM requiring antibiotics. Fortunately, after reviewing the Wispr images with the parents, they left the ED confident that—at this time—their daughter did not have AOM but should make note of the MEE so their primary care physician can make sure it has cleared within three months (which nicely aligned with her 12mo health-maintenance visit).
WiscMed has created a handy visual diagnosis of ear conditions that can be found here.
Here is the complete video exam.

Bullous Myringitis – February 22, 2024
A 7-year-old presented to the emergency department (ED) with severe left ear pain. The pain woke her from sleep and did not respond to a dose of Tylenol, so the child’s mother brought her in for evaluation. She reports her daughter has had congestion but no fever for the past several days. She is otherwise generally healthy with up-to-date immunizations and has no known drug allergies. The physical exam is remarkable for an uncomfortable, crying child. Her Wispr digital otoscope exam is shown.
Which of the following have been implicated in the child’s condition?
- Streptococcus pneumoniae
- Mycoplasma pneumoniae
- Group A Streptococcus
- Respiratory Syncytial Virus (RSV)
- All of the above
Answer: E. All of the above
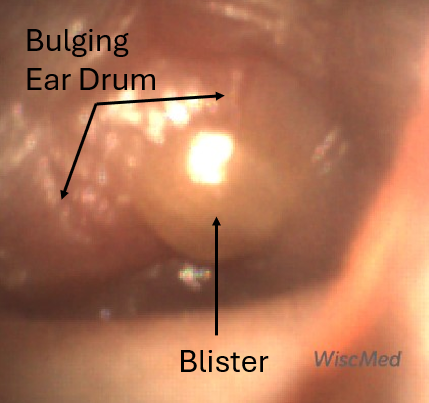
The child has bullous myringitis as evidenced by the impressive blister on her tympanic membrane (TM, ‘eardrum’). Bullous myringitis (BM) is often thought of as a “severe” form of acute otitis media (AOM). BM has bulging and blistering while AOM has bulging without blistering. While an early investigation suggested mycoplasma pneumonia as the most common pathogen, further studies have demonstrated Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, Group A Streptococcus, and Staphylococcus aureus (i.e. the “typical” AOM bacteria) are all frequently isolated when pathology is conducted. In addition, as with many infectious diseases in young children, coinfections with respiratory viruses such as RSV and influenza are common. In a child with no drug allergies and no recent treatment with antibiotics, the American Academy of Pediatrics’ AOM guideline recommends high-dose amoxicillin as the first-line choice for therapy. Bullous myringitis looks painful, and it is. Pain control with oral ibuprofen or Tylenol and topical anesthetic such as proparacaine is important given the severity of ear pain in children with bullous myringitis.
Devaraja K. Myringitis: An update. J Otol. 2019 Mar;14(1):26-29.
Lieberthal et al. AAP Practice Guideline: The Diagnosis and Management of Acute Otitis Media. Pediatrics (2013) 131 (3): e964–e999.
Here is the complete video.

Otitis Media with Effusion – February 15, 2024
An 11-month-old infant presents to the emergency department (ED) with concern for congestion and cough. His parents state the child has been pulling on his left ear, although they note that this is common for him. He has not been crying, fussy, or acting like he is in pain. The family was leaving for a trip in the morning and wanted to be sure, “he was ok” before they got on the airplane. The child had one prior episode of acute otitis media (AOM) three months ago for which he was treated with antibiotics. On exam, there is rhinorrhea with clear lungs and no increased work of breathing. His Wispr digital otoscope exam is shown.
Which of the following is true regarding the child’s condition?
- Treatment with antibiotics is indicated.
- Treatment with decongestants should be considered.
- Treatment with nasal corticosteroids has been demonstrated to be effective.
- None of the above.
Answer: D. None of the above.
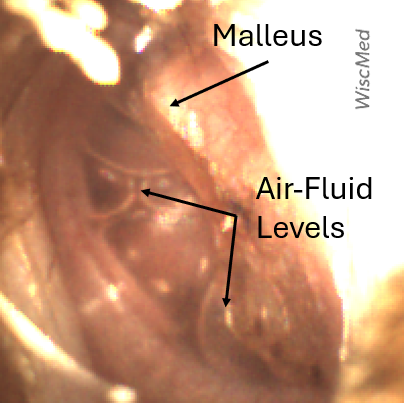
The child’s Wispr exam demonstrates a middle ear effusion (MEE) as evidenced by multiple air-fluid levels. The presence of air-fluid levels without tympanic membrane (eardrum) bulging suggests that the Eustachian tube is properly ventilating the middle ear space. His malleus bone is discernible. His tympanic membrane (TM) does not have moderate or severe bulging nor intense erythema and he does not appear to be uncomfortable. Therefore, the most likely diagnosis is otitis media with effusion (OME). Antihistamines, decongestants, and nasal or systemic steroids are not recommended for treating OME. Since OME can be observed following resolution of AOM or as a precursor to an evolving acute otitis media (AOM), it is important to provide anticipatory guidance for the family. When indicated, this may include just-in-case prescription as well as follow-up to ensure resolution of the OME. This follow-up is particularly important given that persistent MEE may contribute to speech, language, or learning difficulties, and is typically recommended at three months following diagnosis.
WiscMed has created a handy visual diagnosis of ear conditions that may be found here.
Here is the complete video exam. Note how quickly the WiscMed Wispr assists with obtaining a diagnostic view in this 11 month-old.
Reference
Rosenfeld RM et al. Clinical Practice Guideline: Otitis Media with Effusion (Update). Otolaryngol Head Neck Surg. 2016 Feb;154(1 Suppl):S1-S41..

Mucopurulence – February 8, 2024
A 2-year-old child presents to the emergency department (ED) for evaluation of congestion, cough, and low-grade fever over the past 24 hours. The parents are concerned she may have an ear infection since she was recently treated for otitis media with “a pink medicine.” The child finished the full course of antibiotics last week. In the ED, the child is afebrile with normal vital signs and an overall reassuring respiratory examination. Her Wispr digital otoscope exam is shown.
Which of the following is true:
- The child has unresolved acute otitis media and should be started on a different antibiotic.
- The child’s tympanic membrane demonstrates evidence of resolving acute otitis media.
- The child’s tympanic membrane demonstrates severe bulging.
- The child has developed bullous myringitis secondary to acute otitis media.
Answer B. The child’s tympanic membrane demonstrates evidence of resolving acute otitis media.
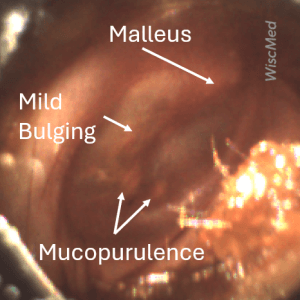
The child in this case has resolving acute otitis media (AOM) as evidenced by only mild bulging and the presence of mucopurulent spots on the anterior inferior quadrant of the tympanic membrane (TM). Mucopurulent spots are from a collection of inflammatory cells adhering to the middle ear surface of the TM. The presence of these spots suggests that the acute phase of the middle ear infection is receding. Here is a 25-day image-series demonstrating the resolution of AOM including the development of the hallmark mucopurulent spots.
The ear drum (tympanic membrane) in this case does not demonstrate severe bulging as the malleus is still discernable.
Bullous myringitis is often thought of as a severe case of acute otitis media. The hallmark of bullous myringitis is severe bulging with blistering on the tympanic membrane. There is no severe bulging or blistering in this case.
Recall that in order to confidently diagnose AOM, the TM should demonstrate moderate to severe bulging. In cases where the TM has only mild bulging (typically occurs in the superior portion of the pars flaccida), the diagnosis of AOM requires either intense erythema or pain—neither of which are present in this child. Mucopurulent material deposited on the inner surface of the TM may occur as the purulent middle ear fluid is cleared during resolution of AOM. This suggests the patient’s TM, while certainly not normal, is not acutely infected and not in need of another course of antibiotics.
WiscMed has created a visual diagnosis guide to common ear conditions which may be found here.
Here is the complete video exam.

Acute Otitis Media – Feb 1, 2024
A 5-year-old female is brought into the pediatric clinic by her mother with concern for right-sided ear pain. The pain began about a day ago and has been managed well with over-the-counter analgesics. Prior to the pain developing, the child had several days of viral symptoms including cough and rhinorrhea. On exam, the child appears unwell, but not toxic. She interacts appropriately. She has a normal temperature and evidence of a runny nose. A frequent cough is noted. The child does not have a history of ear infections. The Wispr digital otoscope exam of her right ear is shown.
What is the next step in management?
- The child has mild acute otitis media (AOM) and a delayed prescription for antibiotics should be considered.
- The child has a middle ear effusion, and no further care is required.
- The child has bullous myringitis and antibiotics should be started.
- The child should be referred to otolaryngology (ENT) for ear tube placement.
Answer 1. The child has mild acute otitis media and a delayed prescription for antibiotics should be considered.
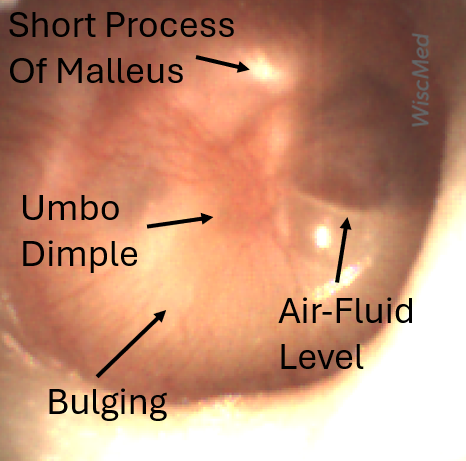
The air-fluid levels present in this image could suggest a middle ear effusion. However, the presence of bulging along with the loss of bony landmarks makes it clear that pressure is building in the middle ear space. Note that only the short process of the normally prominent malleus is visible. When acute otitis media is first developing, it is common to have air-fluid levels as the accumulation of inflammatory fluid in the middle ear starts to displace the air normally found there. Bullous myringitis is a severe form of AOM whose hallmark is blistering of the tympanic membrane.
Based on American Academy of Pediatrics (AAP) guidelines, this presentation of AOM (mild bulging, no fever, pain well-controlled) would be considered either mild or moderate. Compare this case with a case of severe bulging. In a 5-year-old with non-severe AOM, the AAP guidelines are 48-72 hours of observation with a delayed antibiotic prescription. These guidelines can be found here.
Because the child has no history of AOM and the mildness of this presentation, there is no indication for referral to otolaryngology for ear tubes.
WiscMed has created a visual diagnosis guide to the most common ear presentations that can be found here.
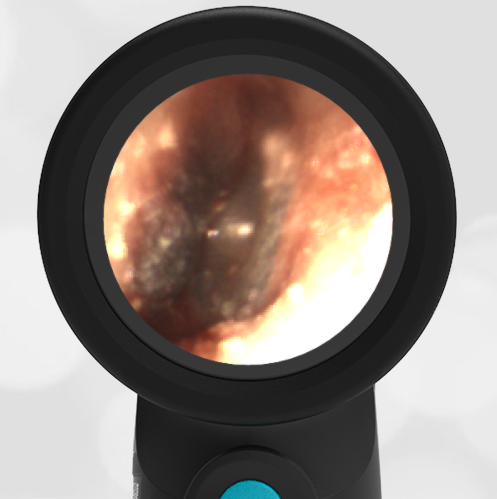
External Ear Canal Bleeding – January 25, 2024
A 7-year-old male presented to the emergency department (ED) with a chief complaint of bloody drainage from his left ear. His father reported the child was in his usual state of health when he went to bed that evening. However, he awoke with blood on his pillowcase and alerted his parents who brought him into the Pediatric ED. The child states he has ear pain. His parents deny any fevers, congestion, or other complaints. He has no prior history of ear infections. He has not been swimming and has no history of eczema or other rashes. He denies trauma but admits to using a Q-tip earlier in the day. His general examination is normal. He has dried blood on his outer ear. He denies tenderness with the manipulation of his external ear.
His Wispr digital otoscope exam is shown.
Which of the following is most likely true of the child’s condition?
- He has acute otitis media (AOM) and should be treated with oral antibiotics.
- He has otitis externa and should be treated with topical antibiotics.
- He has an injury to his auditory canal and topical antibiotics may be considered.
- He has hemotympanum and does not require antibiotics.
Answer: C. He has an injury to his auditory canal and topical antibiotics may be considered.
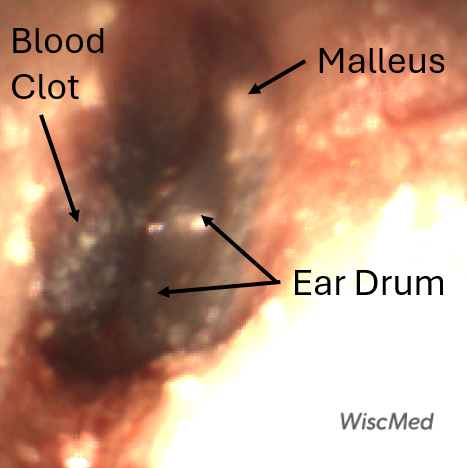
The child has an injury to the external auditory canal (EAC) and topical antibiotics are a prophylactic option. His Wispr exam nicely demonstrates what appears to be a small hematoma versus an area of clotted blood on the inferior surface, just proximal to the tympanic membrane (TM, ear drum). The TM itself appears normal without bulging or other evidence of infection as seen in acute otitis media. The malleus is visible. The EAC is not edematous or inflamed and he has no tenderness with manipulation of the external ear to suggest otitis externa. There is no bloody middle ear effusion as seen with hemotympanum. After further questioning (requiring some gentle probing), the family admitted the “Q-tip” used to clean his ears was a metal loop device. The child states the pain and bleeding occurred after this attempt at removing ear wax and is the obvious culprit in this case of the bleeding ear. Upon follow-up in 24 hours, the child’s ear canal had healed and there was no evidence of significant injury.
Here is the complete video exam.

Extruded Ventilation Tube – January 18, 2024
A five-year-old female presents to her pediatrician for a routine visit. The mother reports that the child has felt well for the past several months. She expresses relief that she has not had to make any emergency visits for ear pain which had been common in the past. During the exam, the following image of the child’s ear was obtained with the Wispr digital otoscope.
Which of the following is true?
- The child placed a bead in her ear which should be removed.
- This object has likely been in the ear for six months.
- Antibiotics should be considered along with hydrogen peroxide drops.
- Referral to ENT is indicated.
Answer: 2. This object has likely been in the ear for six months.

The child has an extruded tympanostomy tube, also known as an ear tube or a ventilation tube. These tubes are inserted across the ear drum in patients that have recurrent middle-ear inflammation, for example from acute otitis media (AOM). Tubes serve to equalize the pressure on both sides of the ear drum. The Eustachian tube normally equalizes pressure across the ear drum. However, in young children, the Eustachian tube is more horizontal than in adults. This makes it susceptible to inflammation which can block its “noodle” like structure and cause pressure to build up in the middle ear. Tubes are placed to relieve the pressure and allow the inflammation fluid to drain.
After about 6 months, the tubes are extruded from the ear drum by the normal action of cell replication. They end up in the ear canal, as seen here. They would normally exit the canal completely in the normal course of daily activities. In this case, there is cerumen (ear wax) that is keeping the tube in the canal. Removal is easily facilitated with forceps.
The extruded tubes can appear like a foreign body. Children are famous for putting items in their ears. Looking closely, it’s clear that this is an ear tube given the cylindrical shape and the flanges on both ends. The eardrum is not seen in this image as the tube is blocking the view. After removal of the tube, the ear can be reinspected for signs of infection. Given the child has no complaints, it is unlikely that she will have ear inflammation and require antibiotics. Hydrogen peroxide drops would only be considered if the tube was still installed in the ear drum and appeared occluded. There is no need to involve ENT in this normal situation.
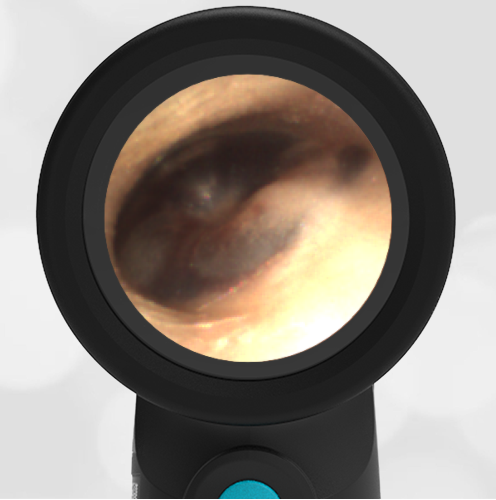
Hemotympanum – January 11, 2024
A 55-year-old female presents to the emergency department (ED) with a bloody nose (epistaxis). Her medical history is significant for chronic liver disease and past admissions requiring transfusions of platelets. She states she suffers from “daily” nose bleeds. This episode started earlier in the day and she has been using nasal packing and pressure to control it. While in the ED she states her hearing is muffled on the left side and requests a hearing test. She has no ear pain, fevers, or other infectious symptoms. She is jaundiced and ill-appearing on exam. Her HEENT assessment is notable for dried blood in the bilateral nares without active bleeding. Her WiscMed Wispr otoscope exam is shown.
What is the likely cause of the patient’s hearing complaints?
- Sensorineural hearing loss associated with chronic liver disease
- Hemotympanum causing conductive hearing loss
- Acute otitis media (AOM)
- Chronic middle ear effusions (MEE)
Answer:
B – Hemotympanum causing conductive hearing loss.
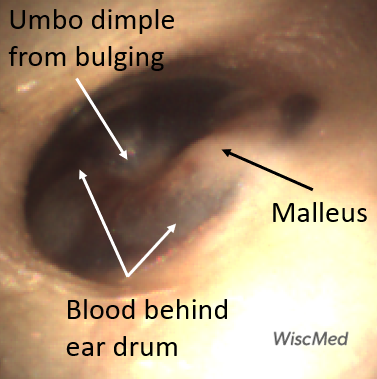
The Wispr exam demonstrates mild bulging and hemotympanum as noted by the bloody-appearing middle ear fluid. The differential diagnosis for hemotympanum includes basilar skull fracture, hemorrhagic otitis media, and ruptured hemorrhagic bullae. However, this patient has no history of injury, ear pain, or fever to support such diagnoses. She does however have chronic liver disease—a risk factor for coagulopathy due to liver dysfunction and splenic sequestration of platelets. Given her physical exam findings and known need for platelet transfusions, the latter is likely the primary factor for her challenging epistaxis history.
Hemotympanum from epistaxis occurs when blood flows retrograde from the nasopharyngeal opening of the eustachian tube (ET) into the middle ear space. While retrograde flow is typically minimized by mucociliary action and a “physiologic valve” whereby the medial portion of the ET is collapsed (ie closed) in the resting state. The opening is controlled by several accessory muscles near the soft palate that are activated by swallowing or yawning and allows equalization of pressure (“clearing the ear, valsalva”). Likewise, nasal packing combined with brisk bleeding can overcome the tube’s protective measures and result in the accumulation of blood in the middle ear space. Here is another example of retrograde hemotympanum.
Both acute otitis media and middle ear effusion are middle ear conditions resulting from inflammation.
WiscMed appreciates the contribution of Dr. James Elliott of the University of Wisconsin for identifying this interesting case.
Szymanski A, Agarwal A. Anatomy, Head and Neck, Ear Eustachian Tube. [Updated 2023 Jun 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482338/
Here is the complete video exam.

Otitis Media or Externa – December 21, 2023
A previously healthy 58-year-old woman contacts her physician-friend with concern for pain just in front of her left ear. She describes the pain as being an ache that seems to localize to the left temporomandibular joint (TMJ). She has no past history of TMJ pain, and she is not diabetic. The discomfort has been getting worse for the past several days. Other than the pain, she has felt well, although she notes that her husband has just come down with Covid. She has tested negative for Covid twice in the past 24 hours. Over-the-counter analgesics have not helped with the discomfort. The following image of her left ear is obtained with a WiscMed Wispr digital otoscope. What is the next step in management?
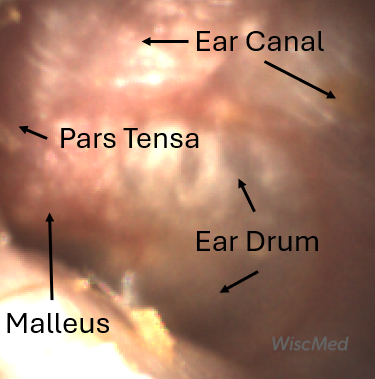 Annotated image
Annotated image
The woman has features of both acute otitis media and otitis externa. The AOM features include bulging of the pars flaccida along with loss of definition of the malleus ossicle. Notably, the pars tensa portion of the ear drum is not bulging and there is no “angry donut” sign. The otitis externa features include inflammation of the external ear canal with erythema. There is no ear canal purulence which is seen with otitis externa.
Definitive diagnosis in this case is difficult. The ear is clearly not normal, but it’s not clear if this is a bacterial infection that requires treatment. Because of the discomfort the patient was experiencing along with mild signs of AOM, she was placed on an oral antibiotic. The next day, she reported the symptoms were not better. She was seen in urgent care and placed on an otic antibiotic drop and instructed to continue her oral antibiotic. Over the course of the following week, the discomfort was much reduced. Ten days later, this image of her left ear was obtained. Note that now the malleus is well-defined, the pars flaccida bulging is gone, and there is no erythema.
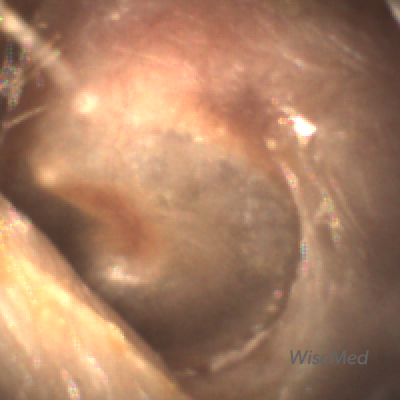
After 10 days of antibiotics
Here are the complete video exams of the initial presentation and post-treatment.
Pre-Treatment Video Exam
Post-Treatment Video Exam
WiscMed has created a visual diagnosis of ear conditions that may be found here.

Normal Ear Drum Features – December 14, 2023
A routine physical exam of a healthy 25-year-old female reveals this image of her left ear drum taken with the WiscMed Wispr Digital Otoscope.
Can you identify at least three anatomical features found in this image?

It’s easy to identify the three bones of the middle ear, the malleus, the incus and the stapes. These are often referred to as the hammer, anvil and stirrup. These three bones transmit the motion of the ear drum to the inner ear where special hair sensors suspended in fluid send electrical signals to our brain that we interpret as hearing.

The cone of light is caused by reflected light from the Wispr otoscope. It is in the anterior-inferior portion of the ear drum with the apex of the cone originating at the umbo of the malleus. The chorda tympani nerve has nothing to do with hearing. It “borrows” the middle ear space to find its way to the posterior of the mouth where it provides innervation for salivation and taste. The promontory is part of the inner ear cochlear apparatus that provides for balance.
Here are images of both the left and right ear.
Here are the complete video exams of the left and right ears.
Normal Left Ear Exam
Normal Right Ear Exam

Cotton Swab Foreign Body – December 7, 2023
A 48-year-old male presents to the internal medicine clinic with concern for a foreign body in his ear. He was using a cotton swab to clean his ear, when the cotton portion of the swab became detached and embedded in his ear.
The attending physician, Dr. Ostrovsky notes “Without the WISPR I would have had to send him to ENT because a simple curette couldn’t snag the cotton and I wasn’t going to fish in his ear with Alligator forceps without some visualization.”
See the video below of the cotton being removed under direct visualization with the WiscMed Wispr digital otoscope.
WiscMed thanks Dr. Daniel Ostrovsky of Duke University Health Systems for this week’s interesting case.

Middle Ear Effusion – November 30, 2023
A 4-year-old child is brought to the emergency department (ED) for evaluation of a bloody nose (epistaxis). His parents note he gets them frequently, but this one did not stop with pressure “like it usually does.” The child has been congested for several days but has not had a fever and denies ear pain. His exam demonstrated a small amount of dried blood crusting the right anterior nasal septum. The child’s Wispr exam of his right ear is shown. The remainder of his exam is unremarkable.
What is the appropriate evaluation and management for this child’s condition?
- He has a middle ear effusion.
- He has mild bulging of the tympanic membrane (TM) and should be given a prescription for antibiotics to fill if needed.
- He has severe bulging of the TM and should be offered immediate treatment with antibiotics.
- The child has hemotympanum, from retrograde nose blood via the Eustachian tube.
Answer: A. He has a middle ear effusion.
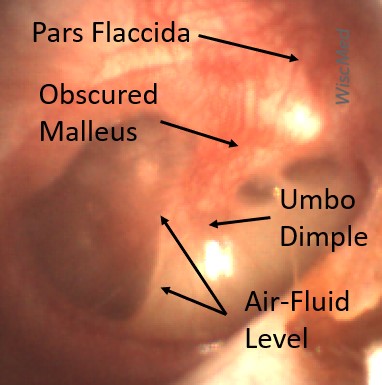
This child has a purulent appearing middle ear effusion (MEE), an incidental finding to the presenting concern of a nose bleed. The initial inclination may be to start treatment for acute otitis media (AOM). However, it is important to not only determine if the findings are sufficient to diagnose AOM, but also if the symptoms are severe enough to warrant immediate treatment with antibiotics.
Research strongly supports using tympanic membrane (TM) bulging as a sensitive indicator of AOM. However, since bulging occurs on a continuum, clinicians must be adept at identifying mild bulging from moderate/severe bulging in order to make a confident diagnosis. The superiorly located pars flaccida is the most compliant portion of the TM and therefore is typically the first area to bulge when pressure increases in the middle ear space. With this early bulging, clear visualization of the bony malleus is impaired and the TM appears “full” with a slight umbo dimple located centrally. As bulging progresses, the central dimple becomes deeper and the malleus more difficult to visualize. With moderate to severe bulging, the deepening dimple results in the appearance of an “angry donut.”
This child’s TM does not demonstrate the donut sign, however, the malleus is not clearly visualized and there is a slight central depression—consistent with mild bulging of the pars flaccida. While mild bulging may be a sign of early AOM, it is also observed with fever, crying, and resolving AOM. Therefore, additional signs or symptoms—either recent onset of ear pain or intense erythema–must be present to diagnose AOM confidently. While there is some injection of the TM, it is not enough to make a definitive diagnosis of AOM and begin immediately initiating antibiotics.
Further supporting the withholding of immediate antibiotics is the lack of symptoms—our patient had no ear pain or fever. It is important to note that once AOM is considered, the actual treatment approach is based on the severity of signs and symptoms. Thus if a diagnosis of AOM had indeed been made based on mild bulging and erythema, the severity would be considered mild. As a child older than 24 months with mild AOM, observation for progression with a delayed prescription would be appropriate.
There is no evidence of blood behind the ear drum (hemotympanum), although retrograde delivery of blood to the middle ear space from a nosebleed does occur as shown in this case.
WiscMed has published a handy acute otitis media treatment poster based on American Academy of Pediatric (AAP) guidelines that may be found here.
Here is the complete video exam.

Bullous Myringitis – November 16, 2023
A 15 month-old-female is brought into the pediatrician’s office with concern for fever and ear-tugging. The child has been in day care where there have reportedly been kids sick with viral symptoms. Yesterday the child became “punky” with a fever of 102.5 F. The parents report that she has been pulling on her left ear. They have been treating the symptoms with over-the-counter analgesics. She does not have a history of ear infections. She continues to eat and drink but with less enthusiasm. On exam, she is an ill, but not toxic appearing child with rhinorrhea and a cough. She appropriately resists the exam. A Wispr digital otoscope provided this image of her left ear.
What is the next step in treatment?
The child has bullous myringitis. This is classified as a severe form of acute otitis media (AOM) with fever. Antibiotics should be started.

The child has the hallmarks of AOM including bulging of the ear drum, loss of bony landmarks, and erythema. In addition, the child has blisters on the ear drum, the hallmark of bullous myringitis. The American Academy of Pediatrics recommends antibiotics for severe AOM which includes temperature above 102.2 F.
The child was started on antibiotics. At a follow-up appointment 3 days later, the eardrum had improved with the blistering resolved. There was still bulging of the eardrum but the child looked much better, and the fever was resolved.
WiscMed has an article on the resolution of AOM over time in images. It can be found here.
WiscMed thanks Dr. Campos for this week’s interesting case.
Here are the complete video exams of the initial presentation and three days post-treatment.
Initial Bullous Myringitis Video
Post 3 Days Bullous Myringitis Video

New Ear Tubes – November 9, 2023
A 33-month-old female presents to the emergency department (ED) for an “ear check.” The child recently had ear tubes placed and has just finished a course of antibiotic drops prescribed by her Otolaryngologist (ENT). She had been doing well until the evening of presentation when she spiked a “fever” to 100.1oF. The family is leaving in the morning for a beach vacation and given her medical history, want to make sure she has not developed another ear infection. The child’s parents deny fussiness, nor have they noted any drainage from either ear. In the ED she is afebrile and has normal vital signs. Her Wispr exam is shown below. The remainder of her general physical exam is unremarkable.
Which of the following is true regarding the child’s tympanic membrane (TM)?
- The tympanostomy (ear) tube is patent and there is evidence of resolving acute otitis media (AOM).
- The child should be sent back to ENT for evaluation of the tympanostomy tube placement.
- There is evidence of recurring acute otitis media and antibiotics should be considered.
- This child should wear earplugs when in the water at the beach.
Answer: A. The tympanostomy (ear) tube is patent and there is evidence of resolving acute otitis media (AOM)
The child has a patent-appearing tympanostomy tube (ventilation, ear tube) that is well positioned. She has no erythema or bulging to suggest an acute otitis media. There are several mucopurulent “mud” spots on both TMs that suggest she recently had otitis media. The tympanostomy tube is flush with the TM and does not require further ENT evaluation.

According to the 2022 American Academy of Otolaryngology-Head and Neck Su
rgery Practice Guideline update, clinicians should not encourage routine, prophylactic water precautions (use of earplugs or headbands, avoidance of swimming or water sports) for children with tympanostomy tubes.
Here is the complete video exam.
Otolaryngol Head Neck Surg. 2022 Feb;166(1_suppl):S1-S55
Still not convinced? Click Here for a Free Trial

Ear Trauma – November 2, 2023
At an otoscopy workshop, a participant presented to the WiscMed station with concern for ear discomfort after a previous ear exam. The Wispr exam of her right ear is shown. What is the source of the participants ear discomfort and what is the next step in management?
The patient has both an old, healed injury to her tympanic membrane (TM) and a new abrasion to her external ear canal (EAC). No further management is necessary.
This is an interesting case because the participant in the workshop has both a healed injury and an acute injury.
The healed injury is to the tympanic membrane, likely from a prior ventilation tube. This healed injury has two features. First is the thinning of the tympanic membrane in the anterior inferior quadrant. This is likely where the ventilation tube had been placed. The thinning is likely due to incomplete healing of a layer of the TM. Second is the sclerosis which is seen as a white patch. Sclerosis is often associated with ventilation tubes or with recurrent acute otitis media (AOM).

Old, Healed Injury
The acute injury is to the external ear canal (EAC). The participant has an area of abrasion to the external ear canal that is causing scant bleeding. The bleeding originates from the EAC and can be seen to flow down the malleus to the central portion of the tympanic membrane. This injury was likely caused by a prior otoscopy exam where the speculum encountered the EAC. This illustrates a key advantage of the Wispr otoscope. The Wispr uses a patented speculum with a unique, small, geometry that makes contact with the EAC less likely, thereby potentially reducing ear trauma.

New, Acute Injury
Here is the complete video exam.
Still not convinced? Click Here for a Free Trial

Ear Canal Osteoma – October 26, 2023
A routine examination of a healthy individual with the Wispr digital otoscope reveals the following image. He has no hearing complaints. He has no ear pain. Which is true of this condition?
- It is a benign growth of bone in the ear canal.
- It is associated with being in cold water.
- Otolaryngology (ENT) consultation on an urgent basis is needed.
- It is usually bilateral.
Answer: 1. It is a benign growth of bone in the ear canal. The patient has an osteoma of the ear canal.

The patient has a benign growth of bone in the external ear canal (EAC). An osteoma is generally unilateral. No treatment is needed unless the growth is so large that it interferes with hearing. Compare an osteoma with exostosis.
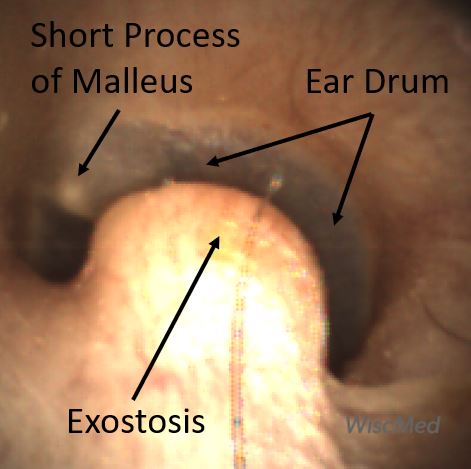
Exostosis

Osteoma
Exostosis is generally found in individuals exposed to cold water for long periods of time. Exostosis is referred to as “surfer’s ear.” Exostosis is usually bilateral where an osteoma is generally unilateral. Exostosis has a more “broad-based” growth to the bone lesion whereas an osteoma often is pedunculated and with an isthmus at its base. In addition, the osteoma is often closer to the tympanic membrane (TM) while exostosis is further from the TM. Neither require treatment unless they become large enough to occlude the EAC.
Here is the complete video exam.
Still not convinced? Click Here for a Free Trial

Bilateral AOM – October 19, 2023
An 8-year-old male with a history of ADHD presents to the emergency department (ED) at 2 a.m. with his mother. She reports that he has a history of ear infections. He’s had mild viral symptoms for the past several days. Last night he began to complain of left ear pain. The mother provided Tylenol and put the child to bed. He woke up with worsening left ear pain resulting in the ED trip. The child is afebrile. He is holding his left ear but is otherwise high-energy and well-appearing. The following image of his left ear is obtained with the Wispr digital otoscope.
What is the next course of action?

Left Ear
The child has acute otitis media (AOM) in his left ear.
The key features include bulging of the tympanic membrane (TM, ear drum), erythema, and loss of the middle ear bony landmarks. In addition, examination of the child’s right ear also reveals mild acute otitis media. Note the difference between the right and left ear. In the right ear (below) the malleus bone is still discernable as the bulging is not yet severe.


Right Ear
WiscMed has created a guide to evaluate and treat acute otitis media based on American Association of Pediatrics (AAP) guidelines. This guide may be found here.
Reviewing the guidelines, the child’s left ear qualifies as severe AOM and should be treated with antibiotics.
Left Ear AOM
Right Ear AOM
Still not convinced? Click Here for a Free Trial

Acute Otitis Media – October 5, 2023
A 20-month-old male presents to the emergency department (ED) with a complaint of congestion for the past three days. Dad reports the child is in daycare and has recently been treated for croup with oral corticosteroids. The child was brought to the ED because overnight he was fussing and said that his right ear “owied.” He received a dose of ibuprofen and was able to return to sleep. In the ED his temperature is 38.5 C, respiratory rate is 32, and Pox 97%. He is overall well-appearing, smiling, and interactive without acute distress or obvious discomfort. The child has mild nasal congestion with clear rhinorrhea, but breath sounds are normal. His Wispr digital otoscope exam is shown.
Which of the following is true of the child’s diagnosis and management?
- The child’s ear is normal.
- The child has exostosis. No further management is needed.
- The child has acute otitis media and should be either (1) treated immediately with antibiotics or (2) offered close follow-up and provided with a delayed antibiotic prescription.
- The child has bullous myringitis and should be prescribed antibiotics with careful return instructions.
Answer C. The child has acute otitis media and should be either (1) treated immediately with antibiotics or (2) offered close follow-up and provided with a delayed antibiotic prescription.

The child has moderate bulging as evidenced by an inability to visualize the middle ear ossicles along with a dimple at the umbo of the malleus. These findings occur due to increased pressure in the middle-ear space from Eustachian tube dysfunction that causes pressure and fluid accumulation. Moderate bulging alone is not enough to diagnose AOM since crying, fever, and Eustachian tube dysfunction may appear similarly. According to the AAP Practice Parameter:
Clinicians should diagnose acute otitis media (AOM) in children who present with moderate to severe bulging of the tympanic membrane (TM) or new onset of otorrhea not due to acute otitis externa.
In this case, the child indicated ear pain that started overnight and was severe enough to interfere with his sleep. Since this would satisfy both the presence of pain as well as an acute onset of the symptom, the patient should be diagnosed with AOM. Of note, the patient’s left ear was normal, see image below.

Normal Left Ear
The treatment options for AOM are dependent on several factors, including a severity assessment and age. In this case, the child appears to have relatively mild severity as his pain (while it woke him up) seems well-controlled with ibuprofen and he has not had a high fever. His left TM was normal; thus, this is a 20-month-old with non-severe, unilateral AOM. According to the AAP Practice Parameter:
Non-severe unilateral AOM in young children: The clinician should either prescribe antibiotic therapy or offer observation with close follow-up based on joint decision-making with the parent(s)/caregiver for unilateral AOM in children 6 months to 23 months of age without severe signs or symptoms (ie, mild otalgia for less than 48 hours and temperature less than 39°C [102.2°F]). When observation is used, a mechanism must be in place to ensure follow-up and begin antibiotic therapy if the child worsens or fails to improve within 48 to 72 hours of onset of symptoms.
After a discussion with the child’s father, he elected to observe for worsening symptoms and arrange for follow-up if needed. A prescription was called into their pharmacy to be filled if the child developed increasing pain, persistent pain, or higher fevers.
Here are examples of a normal ear, exostosis, and bullous myringitis. A normal ear is concave, the middle-ear ossicles are visible and there is a light reflex. Exostosis is a bony growth in the external ear canal that is associated with cold water activities like surfing. Bullous myringitis is a severe form of acute otitis media that presents with blisters on the ear drum.
WiscMed has created a visual guide to ear diagnosis that may be found here.
Here is the complete video exam. Note the power of the Wispr to navigate past ear wax.
Still not convinced? Click Here for a Free Trial

Ear Pain – September 28, 2023
A 3-year-old presents to the emergency department (ED) with a complaint of ear pain for the past several hours. She had previously seemed fine except for a runny nose for the past week. The pain was severe enough to wake her from sleep and she has been crying while waiting in the exam room. In the ED her temperature is 38.5 C, her respiratory rate is 30, and Pox is 98%. She has mild rhinorrhea, but her breath sounds are clear.
Her Wispr exam is noted below.
Which of the following is the primary indication for immediate treatment with antibiotics?
- Fever > 38 C
- Ear pain
- The child’s age
- The appearance of the tympanic membrane (TM)
Answer B – Ear pain

The child has acute otitis media (AOM) as evidenced by severe bulging. While the severity of the bulging is impressive enough to diagnosis AOM, current AAP guidelines utilize illness severity (degree of pain and height of fever), duration, and age as factors in determining when to initiate treatment with antibiotics. When symptoms are severe, age and duration become less important. Therefore, in this case, the presence of severe ear pain would be the primary indication for beginning antibiotics immediately (while also providing adequate pain relief).
The clinician should prescribe antibiotic therapy for AOM (bilateral or unilateral) in children 6 months and older with severe signs or symptoms (ie, moderate or severe otalgia or otalgia for at least 48 hours, or temperature 39°C [102.2°F] or higher).
WiscMed has created a visual diagnosis of ear conditions that may be found here.
Here is the complete video exam.
Still not convinced? Click Here for a Free Trial

Ear Trauma – September 21, 2023
A 4-year-old female presents to her pediatric clinic for ear trauma follow-up. One week ago, the child inserted a thermometer into her right ear. The following image is obtained with the Wispr otoscope.
What is the best course of action?
The child has trauma to her tympanic membrane, likely a perforation. Otolaryngology (ENT) should be consulted. A good starting point for the consultation is sharing this image with them.

The image suggests that there has been trauma to the tympanic membrane (TM, ear drum) just anterior to the umbo of the malleus. A TM perforation is not clearly visible but the area of central darkness suggests congealed blood. In addition, there appears to be blood in the middle ear space, i.e. behind the TM (hemotympanum). The area of trauma to the TM is anterior-superior, likely sparing the ossicles of the middle ear space which are located posterior-superior.
TM perforations often heal on their own. Still, given the age of the child and the likely damage to the TM, an ENT consult on an urgent but not emergent basis is reasonable. The parents should be advised to avoid pool or lake water until an ENT consult is obtained. Antibiotics could be considered but are not generally indicated for a “clean” perforation.
WiscMed thanks Dr. Bradley Harris of Kids First Pediatrics in Scottsboro, AL for this week’s interesting case. Dr. Bradley reports that the Wispr otoscope was particularly helpful in this case as the child was uncooperative. Because of the Wispr’s video capability, there was no need for a nurse to hold the child down during the exam. Here is the complete video exam.
Still not convinced? Click Here for a Free Trial

Otitis Media with Effusion – September 14, 2023
A 32-year-old female presents to urgent care with concern for left ear pain. She has had several days of viral symptoms including cough, congestion, low-grade fever, and fatigue. She has been resting and taking over-the-counter analgesics to manage the symptoms.
A day ago, she began to experience “muffled” hearing in her left ear and a sense of pressure. She has an international trip in two days and wants to make sure she will be able to fly. The image of her left ear taken with the WiscMed Wispr digital otoscope is shown. What is the next step in management for this patient?
The patient has otitis media with effusion (OME). She should be reassured that her symptoms should resolve without intervention and that she is safe to fly.

The hallmark of otitis media with effusion (OME) is evidence of effusion (fluid) behind the ear drum along with air-fluid levels. The malleus bone is identifiable. The air-fluid levels indicate that the middle ear space is being ventilated by the Eustachian tube. This ventilation suggests that with time the effusion should successfully drained to the posterior nasal pharynx. There is no bulging as would be seen in acute otitis media (AOM). No bulging means the pressure on both sides of the tympanic membrane (TM, “ear drum”) is equal. Most likely, this equalization will be able to be maintained in a pressurized commercial airplane where the cabin altitude will be 6,000-8,000 feet. The patient should be encouraged to “Valsalva” as necessary to assist with pressure equalization in the middle ear space.
Compare this case of OME with a normal ear and with the bulging ear in AOM.
WiscMed has created a visual diagnosis guide that may be found and downloaded here.
Still not convinced? Click Here for a Free Trial

Ear Drum Lesion – Sept 7, 2023
WiscMed staff retrieved this image from a customer Wispr that required maintenance. No clinical information is available. WiscMed will provide a $25 Amazon gift certificate to the individual that has the best explanation for the ear drum lesion.
Please send your diagnosis to wiscmedsupport@wiscmed.com. We will update this case with the differential diagnosis answers we receive.

Update September 13, 2023
WiscMed received three responses to this week’s case.
1.
My laptop image is not brilliant, but my initial gut feeling is that it is a man made structure, a hearing aid rubber dome that had some how rotated and been impacted into the anterior recess (pushed in with cotton bud). the central anomaly being the aperture reflecting the majority of light from the otoscope and the malleus is actually light reflex off the side of the dome. I can’t see any real tympanic detail on my laptop image.
Kind Regards,
Steve Mahoney
2.
TM perforated by a Q-tip.
Sandra Lynch
3.
Possible diagnosis: Is this caused by a foreign object, such as a glass bead/diamond that is reflective?
Kind regards,
Christine Richards
Our thought at WiscMed is that this is most likely some kind of cyst. Without additional clinical information, it’s impossible to be more specific. The best course of action would be to send the image to otolaryngology (ENT) and request a consult.
We felt that Dr. Steve Mahoney gave the most complete answer. Thank you, Dr. Mahoney. We will send you the Amazon gift card.
Still not convinced? Click Here for a Free Trial

Acute Otitis Media – August 31, 2023
A 4-year-old female is brought in by her parents to the pediatric clinic. The child has complained of ear pain since last night. Three days ago, she began to experience viral symptoms, including a cough, runny nose, fever and congestion. The parents had been successfully treating the symptoms with over-the-counter analgesics. She appeared to be getting better until the ear pain began. The parents are concerned because her older brother had a history of ear infections and required ear tubes. On exam, the child appears ill without being toxic. She responds well and appropriately resists examination. The image of her painful ear taken with the WiscMed Wispr digital otoscope is shown. What is the next step in management?
The child has acute otitis media (AOM). Antibiotics should be considered.

The hallmarks of AOM include a bulging ear drum, loss of bony landmarks, pronounced vasculature and erythema (redness), and pain. This image clearly demonstrates the physical exam findings of bulging and pronounced vasculature. The umbo dimple is caused by the attachment of the distal portion of the malleus to the ear drum. AOM is often described as looking like an “angry donut.” The bulging is caused by blockage of the Eustachian tube which prevents proper ventilation and pressure equalization across the eardrum in the middle ear space. Antibiotics should be considered for this condition. After initiation of treatment, the pain generally resolves in a day. The physical findings can take up to three weeks to resolve. WiscMed has created a daily visual image series of the resolution of AOM which can be found here.

Myringosclerosis – August 24, 2023
A 4-year-old child presents to the emergency department (ED) for evaluation of cough, congestion, and fever for one day. Due to a prior history of “many ear infections,” the parents wished to have his ears checked prior to leaving for a vacation the following day. The family will be flying out of the country and medical care might not be easily obtained. Upon further questioning, the parents express some concern about their child’s speech development and state their regular physician has mentioned hearing tests. In the ED, the child is afebrile and well-appearing with mild rhinorrhea but no other focal respiratory findings. His Wispr digital otoscope exam is shown.
Which of the following is the most appropriate plan:
- Antibiotics should be prescribed.
- Urgent referral to otolaryngology (ENT).
- Recommend use of a nasal corticosteroid prior to boarding the plane for their trip.
- Recommend follow-up with their primary physician upon returning home.
Answer: D. Recommend follow-up with their primary physician upon returning home.

This child has an impressive amount of myringosclerosis. Myringosclerosis appears as white patches on the tympanic membrane (TM) and results from calcium deposition following repeated episodes of acute inflammation, persistent middle ear fluid, trauma, or tympanostomy tube placement. Despite its appearance, myringosclerosis usually does not impact hearing as long as there is no involvement of the middle ear structures (in which case the term tympanosclerosis is used). It is important to recognize that conditions leading to myringosclerosis (ie persistent fluid or frequent acute infections) can independently contribute to a conductive hearing deficit and may manifest as speech delay. Therefore, children with myringosclerosis and concern for hearing or speech should be followed closely with appropriate ENT referral and audiology testing.
This child’s Wispr exam does not show signs of acute infection—there is no bulging or intense erythema—so antibiotics are not indicated for either acute treatment or expectant management. The child has an upper respiratory illness, so presence of a middle ear effusion (MEE) and Eustachian tube dysfunction are possibilities. However, the degree of myringosclerosis obscuring the normal translucency of the tympanic membrane (TM) makes it difficult to visualize if there are tell-tale air-fluid levels or bubbles behind the TM to suggest otitis media with effusion (OME). Regardless, while there may be some role for newer generation nasal corticosteroids in children with OME and URI symptoms, initiating prior to boarding the plane would likely be of little benefit to the child.
WiscMed has created a visual diagnosis guide to common ear conditions that may be found here.
References:
Pelton, S.I., Marom T. Otitis Media with Effusion (Serous Otitis Media) in Children: Clinical Features and Diagnosis. UpToDate. Retrieved Aug 20, 2023 from uptodate.com
Roditi, R.E., Caradonna, D.S. & Shin, J.J. The Proposed Usage of Intranasal Steroids and Antihistamines for Otitis Media with Effusion. Curr Allergy Asthma Rep 19, 47 (2019)

Otitis Media with Effusion – August 17, 2023
A 2-year-old presents to the emergency department (ED) for evaluation of ear discomfort after his mom noticed him sticking his finger into his right ear. The mom states the child has had several ear infections, the most recent infection being 2 months ago that was treated with antibiotics. Mom reports some concern about his hearing—she notes her son puts his fingers in his ears “a lot” and is lagging behind in his expressive language development. The child has nasal congestion and a low-grade fever but is otherwise well-appearing. The WiscMed Wispr digital otoscope exam is shown.
Which of the following is the most appropriate course of action now?
- The ear is normal, no management is necessary.
- Antibiotics should be prescribed.
- Refer the child to otolaryngology (ENT) for tympanostomy tubes.
- Provide symptomatic relief suggestions and have the child follow up with his pediatrician.
Answer: D. Provide symptomatic relief suggestions and have the child follow up with his pediatrician.
This child has Otitis Media with Effusion (OME) which is defined as middle ear effusion (MEE) without signs of infection of the fluid or inflammation of the tympanic membrane (TM). The hallmarks of OME are air-fluid levels behind a tympanic membrane that is not bulging. Because the TM is not bulging, the malleus ossicle is clearly distinguishable. The fluid is located in the middle-ear space. The lack of bulging and the presence of air along with the fluid suggests that the Eustachian tube is functioning properly.

OME most often occurs as a result of resolving AOM or in association with a viral upper respiratory infection. While typically requiring only supportive care, it should be noted that OME is also at the intersection between resolving AOM, evolving AOM, or Chronic Otitis Media with Effusion (COME), see Diagram 1.
Diagram 1: Relationship of middle ear findings
WiscMed has created a visual ear diagnosis guide that may be found here.
Given mom’s concerns about her child’s hearing, follow-up with the pediatrician is prudent to ensure the fluid does not persist. Current recommendations for ENT referral and consideration for tympanostomy tubes depend on a number of factors including age of the child, duration of MEE, and number of confirmed cases of AOM. The most recent American Academy of Otolaryngology-Head and Neck Surgery guidelines published in 2013 recommend tympanostomy tube (TT) placement for:
1. Bilateral chronic otitis media with effusion (OME) for three months or longer AND documented hearing loss.
2. Unilateral or bilateral OME for three months or longer AND reduced quality of life, ear discomfort, poor school performance, behavioral problems, vestibular problems, or other symptoms that could be attributable to OME.
3. Recurrent acute otitis media (RAOM), defined as three episodes of AOM in 6 months or four episodes in 12 months treated with antibiotics, WITH unilateral or bilateral middle ear effusion at the time of assessment for tube candidacy.
4. At-risk children with unilateral or bilateral OME, which is unlikely to resolve quickly for three months or longer. At-risk children are defined as those with permanent hearing loss independent of OME, speech and language delay, developmental disorders including autism, syndromes or craniofacial disorders which include cognitive, speech, or language delays, blindness or an uncorrectable visual impairment, cleft palate, or developmental delay.
Here is the complete video exam.
Reference:
Rosenfeld RM, Schwartz SR, Pynnonen MA, et al. Clinical Practice Guideline: Tympanostomy Tubes in Children. Otolaryngology–Head and Neck Surgery. 2013;149(1_suppl):S1-S35. doi:10.1177/0194599813487302

Nasal Foreign Object – August 10, 2023
A 3-year-old female is brought into the pediatric clinic by her mother. Earlier in the day at preschool, the child put a bean in her nose. Her mother attempted to remove the bean at home but was unsuccessful.
The following image of her nostril was obtained with the Wispr Digital Otoscope.
What is the next step in management?
The bean needs to be removed from the nostril.
Children have an unlimited capacity to place items in their body cavities.
Examples include beans, beads, tic tacs, pencil tips, erasers, springs, popcorn, and foam.
The bean was removed in the clinic. Techniques to remove the bead include having the mother blow in the non-occluded nostril with the child’s mouth closed, a Katz extractor, glue stick, or forceps. The practitioner generally gets one chance to remove the foreign object in the clinic. After that, the child becomes uncooperative and will often require anesthesia in the operating room to facilitate removal.

WiscMed thanks Dr. Sel Unite of Tree House Pediatrics for this week’s interesting case.

Ear Canal Trauma – August 3, 2023
A mother brings her 3-year-old child to the Emergency Department (ED) with the chief complaint of ear trauma. She states that while attempting to clean the child’s ears with a cotton swab after his evening bath, he jerked away and the swab “went in too deep” in the left ear. The child cried and was upset for several minutes. When he calmed down, Mom inspected the ear and noted blood coming from the canal. Out of fear that she may have permanently injured his ear, she brought him in for evaluation. In the ED, the child is calm and cooperative with the evaluation. His external ear appears atraumatic. The Wispr digital otoscope exam of his left ear is shown.
What action needs to be taken?
No further action needs to be taken.
This child has an injury caused by a common mechanism with a household item. The Wispr exam demonstrates bleeding in the external auditory canal (EAC) with a small amount of bright blood pooling near the base of the tympanic membrane (TM, ear drum). The TM itself does not appear acutely injured as there is no obvious perforation, excoriation, or injection. Careful return instructions should include increasing pain, fever, or decreased hearing.

The innocuous-appearing cotton-tip applicator (cotton swab) accounts for thousands of ED visits each year, with 2/3 of the injuries occurring in children under 8 years of age. Most injuries are either TM perforations or, as in this case, external ear canal (EAC) abrasions. While there exists a myth that waxy ears equal dirty ears, this is contrary to the message put forth by the American Academy of Otolaryngology-Head and Neck Surgery Foundation. Its list of do’s and don’ts for patients includes “Do know that ear wax is normal” and “Don’t put cotton swabs, hair pins, car keys, toothpicks, or other things in your ear.” In other words, while cerumen may be an annoyance to all those attempting to evaluate a young child’s TM, care ought to be taken to dispel the misconception that cleaning out the ear canal ought to be a routine part of bath time.
Here is a complete video of the exam:
Source:

Foam in Ear Canal – July 27, 2023
A 5-year-old male is brought to the pediatric clinic by his parents for a well-child visit. The parents describe him as a healthy, active, and curious child. They have no specific concerns about this visit. During the exam, this image of the child’s right ear canal was obtained with the Wispr digital otoscope.
What question would you ask the child and his parents?
The child has a piece of foam in his ear canal. The question to ask the child or his parents is if they know where this came from.
As is typically the case, the child and the parents have no memory of this foreign object being placed in the ear. Oftentimes, it is a sibling or even a pet who “thoughtfully” places the foreign object in the ear canal.
This is a common clinical scenario. An incidental finding of a foreign body in the pediatric ear canal. In this case, the child did not recall placing something in his ear. Removal of this foreign body could be accomplished easily with forceps.
Children are famous for putting objects in their ears. Objects commonly seen include beads, beans, earrings, pencil tips, Tic-Tacs, and popcorn. Also often found in the canal are insects such as ants, spiders, and flies.
WiscMed thanks Dr. Laura Luckadoo of The Childhealth Center for this week’s interesting case.

Tympanostomy Tube – July 20, 2023
A 45-year-old male with a history of middle ear infections presents to the ENT clinic for a follow-up appointment. He had a ventilation tube placed 12 months ago. He has no current concerns.
What do you notice that is unique about the tympanostomy tube in this image taken with the WiscMed Wispr digital otoscope?
This is a “long term” tympanostomy tube and may be occluded.

Tympanostomy (ventilation, ear) tubes are placed to drain fluid from the middle ear space. Commonly this is done for children that have recurrent acute otitis media. Adults generally don’t get middle ear infections because their eustachian tubes drain more vertically to the posterior nasopharynx. In this case, the patient appears to have had a long history of middle ear infections as the tympanic membrane appears sclerosed. This ventilation tube is interesting because it is a long-term tube; the tube is longer and it does not have an external flange. Both of these features help to prevent the extrusion of the tube. Compare this long-term tube with a more typical pediatric tube. Note the external flange on the short-term tube.
This tube also appears to be occluded. If the tube is blocked, ventilation of the middle ear space is not occurring. This suggests that the tube either needs to be replaced or an attempt should be made to unblock the tube.
Here is the complete video exam:

Bullous Myringitis – July 13, 2023
A colleague asks you to consult on a tympanic membrane image obtained with the Wispr digital otoscope. To challenge you, your colleague does not provide you with any clinical information. Which of the following statements is most likely true?
- This is a young child who has had several days of viral symptoms.
- This is an individual that is exposed to cold water frequently.
- This patient requires urgent consultation with otolaryngology (ENT).
- There is no indication for treatment at this time.
Answer: 1. This is a young child who has had several days of viral symptoms.
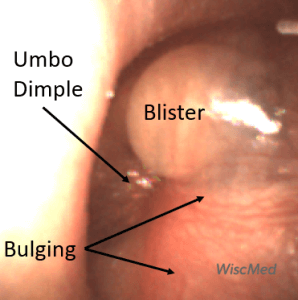
The child has bullous myringitis (BM). Classically a child with BM will present with several days of viral symptoms such as cough, congestion, and fever. The viral infection can lead to Eustachian tube dysfunction which allows for a bacterial infection to develop in the middle ear space. BM can be considered to be a variation of acute otitis media. Bullous myringitis includes the hallmarks of AOM including bulging, an umbo dimple, loss of bony landmarks, and erythema (redness). In addition, bullous myringitis is distinguished from AOM by the presence of blistering on the tympanic membrane (TM, “ear drum”). Antibiotics would be strongly considered as a treatment for bullous myringitis, just as they are for acute otitis media.
Historically, bullous myringitis was thought to be caused by Mycoplasma pneumonia. However, as Mellick (1) shows in his letter, it is a component of severe AOM whose underlying cause may be a number of infectious agents.
An individual that is exposed to cold water frequently can develop exostosis. Exostosis is an overgrowth of the bony ear canal. The difference between exostosis and bullous myringitis is easy to appreciate. BM has bulging, blistering on the TM and it looks “angry.” Exostosis has a non-infectious bone growth on the canal.
Compare BM and exostosis side-by-side:
An example of an urgent consult to ENT would be a cholesteatoma. This is an overgrowth of the cells behind the TM. A cholesteatoma can be distinguished from BM because the TM does not look angry and there is no bulging. A cholesteatoma needs evaluation and potential treatment as it can erode the ossicles in the middle ear space and cause hearing loss.
Compare BM and a cholesteatoma side-by-side:
WiscMed has created a visual diagnosis guide to common ear conditions. The guide may be found here.
(1) Mellick and Verma, Letter, Pediatric Emergency Care, Volume 26, Number 12, December 2010

Ear Canal Polyp – June 29, 2023
A healthy 35-year-old male presents to internal medicine for a routine clinic appointment. He has no complaints. Evaluation of his left ear with the Wispr digital otoscope produces this image. What is the next step in management?
The patient has a polyp in his ear canal (aural polyp). Consultation with otolaryngology (ENT) is appropriate.

This abnormal growth is likely not cancerous. It may be from localized inflammation from irritation, a tumor, or a vascular abnormality. It is likely painless and would not come to medical attention unless it grew to obstruct the ear canal or it began bleeding. ENT should be consulted non-emergently, starting with this image, for definitive management.

Acute Otitis Media – June 22, 2023
A 4-year-old female is brought in by her mother to the pediatric clinic. The child has been complaining of right ear pain for a day. The mother indicates that the child had several days of viral symptoms including cough, runny nose, and temperatures to 100.5 F. Yesterday, the child began pulling at her right ear and complaining of pain. The child has a history of “ear infections”. The mother has been treating the symptoms with over-the-counter analgesics.
On exam, the child is afebrile with rhinorrhea. She is alert and cooperative but appears “punky.” She says her right ear hurts. This image of her right ear is obtained with the Wispr digital otoscope. What treatment is indicated?
The child has acute otitis media (AOM). Antibiotics should be considered.

This Wispr otoscope image demonstrates all the hallmarks of an ear infection. There is bulging of the tympanic membrane (ear drum) and the umbo dimple is present due to the bulging. Bony landmarks are lost as there is only the hint of the lateral process of the malleus bone. In addition, there is pronounced vasculature of the eardrum leading to an erythematous (red) appearance. Compare this case of AOM with a normal ear. The normal eardrum has no bulging, is concave, it is not red, and the bones of the middle ear are easily appreciated.
The case presented here is “classic.” The prodrome of AOM is often a viral infection. This infection leads to Eustachian tube dysfunction which creates an environment where bacterial infection and inflammation produce fluid in the middle ear space. Because the Eustachian tube is not functioning, the fluid creates pressure in the middle ear space resulting in bulging of the ear drum. The symptoms of this bulging include pain and decreased hearing. Antibiotics should be considered for this condition. If the child continues to have recurrent ear infections, ventilation tubes may be considered. Ventilation tubes are placed thru the tympanic membrane to drain and ventilate the middle ear space.
WiscMed has produced a visual guide to ear conditions that may be found here.

Foreign Object – Eraser Tip
June 15, 2023
A healthy 6-year-old boy arrives with his mother for a wellness check at his pediatric clinic. The child has been doing well and the mother has no concerns.
During his physical exam, this image of his ear was obtained with a Wispr digital otoscope.
What is your diagnosis and plan of action?
The child has an eraser tip in his ear. Removal of the eraser is indicated.

This is a remarkably common clinical scenario. An incidental finding of a foreign body in the pediatric ear canal. In this case, the child did not recall placing something in his ear. Removal of this foreign body could be accomplished easily with forceps or a curette. Children are famous for putting objects in their ears. Objects commonly seen include beads, beans, earrings, pencil tips, tic-tacs, and popcorn.
WiscMed thanks Dr. Laura Luckadoo of The Childhealth Center for this week’s interesting case.

Waxy Ear
June 8, 2023
A fussy 12-month-old is brought to the Emergency Department (ED) by his mother who is concerned her son has an ear infection. He has been evaluated in the past for similar complaints of pulling at his ear and recently completed a course of antibiotics. That evening he seemed more irritable and had been pulling at his right ear. His parent states he has “a lot of wax” and exams have been difficult. The child is afebrile and well-appearing.
The Wispr digital otoscope exam of his right ear is shown.
Does this child have an ear infection?
No. The child’s tympanic membrane (TM) is normal.

The child’s tympanic membrane (TM) is not bulging and has a normal appearance of bony landmarks and light reflexes. There are prominent blood vessels (vasculature) at the superior aspect of the TM. This is a normal finding in a crying child. Mom was correct in stating her child had “a lot of wax.” Compare this normal TM image with a case of acute otitis media (AOM). Without the Wispr digital otoscope, it would not have been possible to obtain this full view of the TM. The Wispr’s unique speculum geometry and camera location allow for a full view of the TM even in largely occluded canals.
See the complete video below to observe how the Wispr can use a small window in the wax to get a beautiful view of the normal TM.

Foreign Body?
June 1, 2023
A healthy 30-year-old male presents to urgent care with concern for decreased hearing in his right ear. He says it seems like his hearing has been gradually getting worse for a few weeks. There is no pain, but a sensation of “fullness.” He has no history of ear trauma or infections. The following image of his right ear is obtained with a Wispr digital otoscope. What is the next step in management?
The patient has an object in his ear canal.

The object appears to be an almond, but there is no history from the patient to suggest this is the case. A curette was used to gently remove the object. The object was a piece of congealed cerumen (ear wax). This case is interesting because cerumen does not usually form a shape like this. Cerumen usually is diffusely organized and tends to layer inferiorly due to gravity. It can also take on a transparent appearance as this previous case shows.
Cerumen is not a foreign object as it is a natural part of the body’s defense mechanism. Examples of true foreign bodies include ants, ticks, flies, pinto beans, pencil tips, earbuds, and earrings.
WiscMed has published a visual guide to common ear conditions. This guide can be found here.

Incudomalleolar Joint – May 25, 2023
A healthy adult pediatrician visited the Pediatric Academic Societies WiscMed booth for a demonstration of the Wispr digital otoscope. She has no history of ear trauma or infections. She has no ear complaints. The following image of her right ear is obtained with a Wispr digital otoscope.
What unusual feature do you notice about the middle ear bones (ossicles)?
The incudomalleolar joint is partially visible.

There are three ossicles in the middle ear, the malleus, incus, and stapes. The bones are visible to otoscopy due to the semi-transparent nature of the tympanic membrane (TM). The first bone, the malleus, is easily visible except in cases of anatomic distortion, for example from acute otitis media (AOM). The second bone, the incus, is visible sometimes. The third bone, the stapes, is the deepest of the middle ear bones, and only occasionally can it be seen by otoscopy.
The unique observation in this patient is that the inferior portion of the malleus-incus (incudomalleolar) joint is visible. This is unusual as the joint is usually superior to the external ear canal. In this case, the patient has pseudo retraction of the pars flaccida portion of the TM. Because of this, there is an unusual opportunity to appreciate the joint.
Here is the video of the complete ear exam:

Middle Ear Effusion – May 18, 2023
A 10-month-old female presented to the emergency department (ED) with concern about an ear infection “that is not getting better”. She was seen two weeks ago and completed a course of antibiotics, but has continued to stick her fingers into both ears. Mom interprets this behavior as indicating pain and is worried because she has already been on antibiotics four times for ear infections.
In the ED, the child was afebrile and well-appearing. However, when approached for the otoscopic examination, she immediately started to cry and became extremely upset. Despite being less than cooperative, the Wispr digital otoscope captured the following image of her left tympanic membrane (TM).
What is the next step in the management of this patient?
The child has a middle ear effusion (MEE). No additional management is required.

The child’s Wispr exam clearly demonstrates the presence of middle ear fluid, with air-fluid levels noted behind translucent TMs. Even though the fluid appears milky, the TMs are not bulging nor do they appear inflamed with marked injection. In fact, the malleus is prominent which indicates the pars flaccida is retracted, likely due to negative middle ear pressure associated with resolving acute otitis media (AOM). The presence of MEE and the negative pressure may be causing the child to “stick her fingers in her ear” but they do not indicate an acute infection, thus she does not need to be on another course of antibiotics.
Mom expressed concern about the previous antibiotic prescriptions and the challenges encountered during the ear examination. A review of the child’s electronic medical record (EMR) was performed to better understand her medical history. One note provided the medical decision-making for at least one of her prescriptions (paraphrased): “The child was fussy and uncooperative during the ear exam, limited view but TMs seemed red.” It is unknown if the child did indeed have TM bulging at this visit, however, the documented physical findings as well as the child’s challenging exam (which was clearly on display in the ED) do not seem to indicate the need to immediately start antibiotics. Many clinicians will agree that this is an unfortunate and all-too-familiar scenario with regard to identifying the source of fussiness or fever in an uncooperative child. Overcalling AOM due to lack of access to the TM results in unnecessary antibiotics, expense, and worry and can detract from identifying a more serious etiology for the child’s fever. Fortunately, Wispr digital otoscopy is providing clinicians with a tool to address this challenge and improve diagnostic certainty. In this case, the combined otoscopic examination time for both ears lasted ten seconds and allowed the child’s parent and the clinician to be confident in the diagnosis and to avoid another course of unneeded antibiotics.
WiscMed has published a visual guide to the diagnosis of common ear conditions that can be found here.
Here are the complete video exams of the left and right ear. Both demonstrate MEE.
|
Left Ear |
Right Ear |

Exostosis – May 11, 2023
A pediatric resident brought her father to visit the WiscMed booth at the Pediatric Academic Societies (PAS) 2023 annual conference. He is a 75-year-old gentleman with no hearing complaints other than occasional difficulty “hearing my wife.” He told WiscMed staff that he had been told he had an “interesting” finding in his left ear. He has been aware of the “finding” for a long time.
The Wispr digital otoscope image of his left ear was obtained.
What is your diagnosis?
The gentleman has exostosis of the left ear canal. No action is necessary.

Exostosis is a benign growth of bone, in this case in the ear canal. It is a common finding and generally of no clinical significance. Classically, exostosis is associated with cold water exposure, such as surfing. Prolonged exposure to cold seawater is thought to induce an inflammation cascade that results in osteoblast activity. This individual did not have a history of repeated exposure to cold water. Exostosis can be mild, moderate, or severe depending on how much of the external canal is blocked. If exostosis is severe enough, it can cause hearing loss and make the ear susceptible to otitis externa. In those cases, surgical removal of the bony overgrowth may be required.
Further information on exostosis may be found here.
Here is the video of the complete ear exam:

Wax Annulus – May 4, 2023
A healthy 40-year-old male presents to internal medicine for a routine physical exam. He has no concerns about today’s visit. The following image of his left ear is obtained with the Wispr digital otoscope. What is your diagnosis, and what is the next step in management?
The patient has a ring of cerumen (wax) lying inferiorly. No further action is necessary.

This is an interesting image. At first glance, it appears to be a tympanic membrane rupture. However, it is simply cerumen (wax) layering inferiorly. The cerumen in this image has a lighter and almost transparent appearance that makes it look like it could be the tympanic membrane, and thus a rupture. Actually, the cerumen is lying inferiorly from about the 10 o’clock to 3 o’clock position. There also appears to be a partial ring of cerumen that is deeper at the 11 o’clock to 3 o’clock position.
This digital image allows time to realize that the expected features of the tympanic membrane are present and undisturbed. These features include the malleus and incus, the cone of light, and the Eustachian tube (ET) shadow. This is an uncommon appearance of cerumen. Generally, ear wax appears more yellow.
Here is the video of the complete ear exam:

Mild Bulging AOM – April 27, 2023
A 7-year-old presents to the emergency department (ED) with right ear pain for one day. The pain started earlier in the evening and kept her awake, so her mom brought the child in for evaluation. Aside from ear pain, she has otherwise been well without fever, cough, or other respiratory complaints. The child has not been swimming recently and the mom does not report any ear drainage. Her mother states the child used to have frequent ear infections but has done much better since tubes were placed several years ago. Immediately prior to the examination, the child stated, “I just felt my ear pop and now the pain is better.”
Her Wispr digital otoscope exam is shown.
Which of the following is true regarding this child’s presentation?
- The tympanic membrane (TM) is normal, and no antibiotics are indicated.
- The TM demonstrates a middle ear effusion (MEE), and no antibiotics are indicated.
- The TM demonstrates mild bulging and antibiotics may be prescribed “as needed” if symptoms worsen.
- The TM demonstrates severe bulging and immediate initiation of antibiotics is indicated.
The answer is 3, The TM demonstrates mild bulging and antibiotics may be prescribed “as needed” if symptoms worsen.
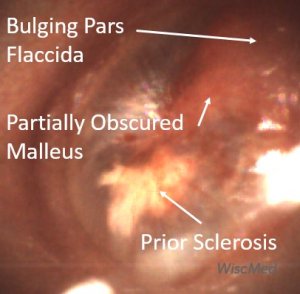
The child’s TM demonstrates mild bulging as evidenced by the bulging in the pars flaccida region that obscures the visualization of the malleus and distorts the normal light reflex. The TM has not progressed to severe bulging which would take on the appearance of a deeper central depression (i.e. donut sign). The child’s TM also has erythema, particularly centrally where small hemorrhages are noted. The white patch (sclerosis) noted in the posterior inferior quadrant is likely a result of her prior ventilation tube placement. According to the American Academy of Pediatrics (AAP) practice parameters for diagnosis and management of acute otitis media (AOM):
Clinicians should diagnose AOM in children who present with mild bulging of the TM and recent (less than 48 hours) onset of ear pain (holding, tugging, rubbing of the ear in a nonverbal child) or intense erythema of the TM.
Given this definition as well as the child’s initial complaint of pain that brought her into the ED, one could argue for immediate initiation of antibiotics. However, given the child’s age (able to communicate clearly about her symptoms) and the improvement in her pain after her “ear popped” (suggesting her Eustachian tube opened and relieved some of the pressure), a reasonable course of action is to continue to address comfort and provide a “just in case” antibiotic prescription if her symptoms worsen over the next 48 hours. Despite pain relief and ear popping, there are no air-fluid levels present to suggest a middle ear effusion.
Here are examples of the ear conditions represented by the answer choices listed above.
Watchful waiting management of acute uncomplicated AOM is supported by the AAP guideline. However, there appears to be resistance among clinicians to this approach as a recent review of the management of acute uncomplicated AOM demonstrated a high antibiotic prescription rate, particularly among non-otolaryngologists. The rationale for these differences remains to be determined, but uncertainty in diagnosis likely plays a role in the hesitancy of clinicians to defer antibiotic initiation. As can be observed in this child’s case, a very clear image of the TM allows conversation with the parent and provides confidence in the decision. After reviewing the images of her child’s TM, discussing how her child’s findings differ from that of certain AOM, and providing alternative strategies for management, the mother was very happy to defer antibiotics—while also feeling empowered to fill the prescription if the symptoms worsened.
WiscMed has created a visual diagnosis guide to common ear conditions that may be found here.
Here is the video of the complete ear exam:
Lieberthal A, Carroll E, Chonmaitree T et al. The Diagnosis and Management of Acute Otitis Media. Pediatric, Mar 2013; 131(3).
Slominski N et al. Watchful Waiting for Acute Otitis Media. Pediatrics (2022) 150 (1).

Cholesteatoma – April 20, 2023
A healthy 24-year-old female presents to the internal medicine clinic for a routine checkup. She has no specific concerns about this visit. She has no hearing complaints. She has no history of ear infections or ear trauma. The following image of her ear is obtained.
What is true about this image obtained with the Wispr digital otoscope?
- This is a congenital finding of no significance.
- She likely has a history that includes cold water activities such as surfing.
- She requires an otolaryngology (ENT) evaluation.
- This is bullous myringitis.
Answer 3. She requires an otolaryngology (ENT) evaluation.

The patient has an anomaly in the posterior-superior area of her tympanic membrane (TM). This anomaly appears to be deep in the TM. The classic lesion occurring deep in the TM is the cholesteatoma. A cholesteatoma is an overgrowth of cells behind the tympanic membrane that can erode the ossicles (bones) of the middle ear and cause hearing loss. Note how close this lesion is to the incus and stapes bones and the chorda tympani nerve. Because of the possibility of destruction to these structures, otolaryngology (ENT) should be consulted. Cholesteatomas may be either congenital or acquired. While this patient’s lesion has had the appearance of a possible cholesteatoma, its location is atypical. Congenital cholesteatomas are typically in the anterior-superior quadrant. Cold water activities such as surfing are associated with exostosis which is a benign bony outgrowth of the ear canal. Bullous myringitis is an infection of the middle ear space (acute otitis media), whose hallmark includes blistering of the TM.
WiscMed has created a visual diagnosis guide that can be found here.

Resolving AOM – April 13, 2023
A 20-month-old presented to the emergency department (ED) due to concern about an ear infection. Mom reports her daughter has “chronic” nasal congestion and was treated a month ago for acute otitis media (“again!”). The child has not reported any ear pain, but her mom noted her “sticking her finger in her ear today.” She has had no recent fevers. She is otherwise well appearing with an unremarkable exam. Her Wispr digital otoscope exam is shown.
Which of the following is true regarding the child’s ear findings?
- The child has a profoundly bulging tympanic membrane (TM). Antibiotics are indicated to treat her acute otitis media (AOM).
- Sclerosis is present.
- The white patch at the 8 o’clock position is a result of a resolving ear infection.
- The child has an erythematous (red) TM. An urgent consult with ENT is indicated.
The answer is 3. The white patch at the 8 o’clock position is a result of a resolving ear infection.

The child’s tympanic membrane (TM) is mildly bulging as evidenced by the loss of boney landmarks and the presence of a depression/dimple in the central TM where the fixed attachment of the umbo is located. The TM does not have the classic “donut” appearance that is characteristic of moderate to severe bulging, thus acute otitis media (AOM) cannot confidently be diagnosed. There is some purulent appearing material that is adherent to the inner TM surface. At the 8 o’clock and 10 o’clock positions, this material has coalesced into patches. These patches are common findings in children with frequent AOM and are typically found one to eight weeks post-infection. They are thought to be from residual debris associated with the AOM inflammation cascade. Their presence is a hint of a resolving ear infection. Sclerosis is often present after ear infections or ear tube placement. However, in this case, there is no evidence of sclerosis. If you look closely, erythema near the periphery of the patches can be distinguished as blood vessels. These “sentinel vessels” likely are also responses to the inflammation in the middle ear and are another characteristic finding of resolving AOM.
Compare the following; a normal ear, this week’s case, and a severe case of acute otitis media.
The mother should be given return instructions in the event of ear pain or fever.
WiscMed has created a visual diagnosis guide to common ear conditions. This guide can be found here.
Here is the complete video exam:

Chronic Changes – April 6, 2023
A 60-year-old male presents to the clinic for a re-evaluation of his left ear. Two weeks ago, he was seen in the clinic and was diagnosed with a viral infection and a left ear infection. He completed a course of prescribed antibiotics. Both his viral symptoms and his ear pain have improved.
The Wispr otoscope exam of his left ear is shown here.
What is the next step in management?
The patient has chronic-appearing changes to his left ear. No further action is necessary.
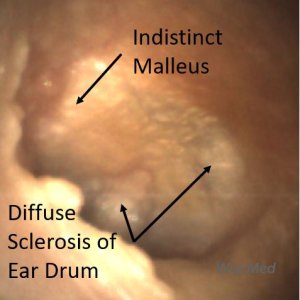
The patient has what appears to be chronic changes to his left ear. The malleus is indistinct and there is evidence of of the ear drum. Compare a normal ear, this image of chronic changes, and an ear with acute otitis media (AOM).
Although the malleus is indistinct in the chronic change image, it is present and discernable unlike in the case of AOM. In addition, there is no bulging of the ear drum as in the AOM example. The chronic tympanic membrane is clearly not as pristine as in the normal case. It’s easy to imagine that the ear drum with chronic changes has experienced multiple insults (infections, trauma) that have resulted in the scarred appearance.
Given the appearance of the ear in this week’s case, it calls into question if there was in fact an ear infection present two weeks ago. It’s possible that with a quick and incomplete glance using an analog otoscope that the chronic changes may have appeared acute. Here is an article on the natural history and resolution of an ear infection in images. Note that it takes many weeks for a case of AOM to completely resolve.
WiscMed has prepared a visual diagnosis guide to ear conditions that may be found here.
View a video of the complete ear exam:

Healthy Tympanic Membrane – March 30, 2023
A healthy 25-year-old male with no complaints sees his primary care physician for a routine checkup. This image of the patient’s ear is obtained.
He asks you to explain what he is seeing in the image.
What structures can you outline for this curious patient?

This is a nice example of a healthy and normal tympanic membrane (TM). The most obvious structures are the three bones of the middle ear, the malleus, incus and stapes. These three bones are actually “behind” the tympanic membrane. They are visible because the TM is a thin and partially translucent membrane. Their purpose is to translate and amplify the vibration of the eardrum to the inner ear. The malleus is connected to the incus superior to what is visible through the TM. It is unusual to be able to see the most distant bone, the stapes, as it tends to be further away from the TM.

In addition to the bones of the middle ear, the Chorda Tympani nerve is also visible. This nerve runs behind the malleus and in front of the incus. It has nothing to do with sensation or motor to the ear. It borrows this convenient middle ear space as it makes its way to the tongue to provide taste sensation and innervation to the sublingual and submandibular glands in the mouth. The Eustachian tube shadow is the opening of the Eustachian tube in the middle ear. This tube connects the middle ear to the posterior nasopharynx. Its job is to equalize pressure on both sides of the TM. Its function is familiar to us as it allows our ears to “pop” during the descent of an airplane.

Blocked Ear Tube with AOM – March 23, 2023
A 6-year-old female is brought to the pediatric clinic by her mother with concern about ear pain. The child has had 3 days of viral symptoms including fever, cough, and runny nose. Yesterday, the child began to have right-sided ear pain. The mother has been managing the symptoms with an over-the-counter analgesic. The child has a history of ear infections. Six months ago, ventilation tubes (ear tubes) were placed to manage recurrent infections.
The child’s Wispr otoscope exam is shown. What is the appropriate intervention?
- The ventilation tube should be mechanically cleared.
- No intervention is necessary, this will spontaneously resolve.
- Antibiotics should be considered along with hydrogen peroxide drops.
- Blockage is almost always caused by an accumulation of cerumen (ear wax).
The answer is 3. Antibiotics should be considered along with hydrogen peroxide drops.
The child has an occluded tympanostomy (ear, ventilation) tube with evidence of acute otitis media (AOM).

Ear tubes are placed in the tympanic membrane to drain inflammation fluid from the middle ear space. This inflammation is from infections, often with a prodrome of viral symptoms. If the tube becomes clogged, fluid no longer drains from the middle ear, and pressure (bulging) and discomfort increase. In this image, the annulus of the tube is clearly obstructed. In addition, there is evidence of broad bulging of the ear drum, especially in the pars flaccida region. The bulging has almost completely obscured the malleus bone. Younis(1) has published a guide to managing plugged tympanostomy tubes. Dr. Younis notes that the plugging material is generally from the inflammatory middle ear fluid, not cerumen. Attempting to mechanically clear the tube is painful, traumatic, and generally not successful. Hydrogen peroxide drops clear the blockage 85% of the time. Because there is evidence of AOM in this case, antibiotics should be considered.
WiscMed has published a visual diagnosis guide to common ear conditions. This guide can be downloaded as a pdf here.

Acute Otitis Media with Scant Erythema
A 4-year-old previously healthy male is brought to the pediatric clinic by his mother. The child has had 3 days of cough, congestion, and fever. Yesterday, he began to develop left ear pain. His mother has been treating the symptoms with over-the-counter analgesics.
On exam, he is an active young man with a cough and runny nose. His temperature is normal. This image is obtained with the Wispr digital otoscope.
What is your diagnosis and what action should be taken?
The child has acute otitis media. Antibiotics should be considered.

The hallmark of acute otitis media (AOM) is the bulging ear drum, as seen in this case. The bulging is caused by increased pressure due to inflammation in the middle ear space. The appearance is often described as an angry bagel. The dimple in the middle is caused by the attachment of the umbo which is the distal portion of the malleus ossicle. Generally, there is intense erythema (redness) associated with an ear infection. The erythema is caused by increased vasculature along the tympanic membrane. What is interesting about this case is that scant erythema is present. Despite this, the vasculature is quite pronounced. Compare this case of AOM to a normal ear shown here.
WiscMed has published a visual diagnosis guide to common ear conditions. This guide can be downloaded as a pdf here.

Middle Ear Effusion with Cerumen
A 17-month-old presents to the emergency department (ED) with concern about an ear infection. The child had a runny nose and mild cough for several days and developed a fever on the evening of the presentation.
Aside from being treated the previous month for an ear infection, he is otherwise generally healthy and has not been pulling at his ears.
In the ED, he is a happy toddler with nasal congestion and a reassuring respiratory exam. His right ear Wispr exam is shown below.
What treatment is indicated?
The child has a middle ear effusion (fluid behind the eardrum). No treatment is indicated.

While not a normal appearing tympanic membrane (TM), this child does not have an ear infection, acute otitis media (AOM). His exam is consistent with a middle ear effusion (MEE) and does not require antibiotics at this time. Findings that support this assessment are the lack of TM bulging, no intense erythema (redness) of the TM, and no concern for a painful ear. In addition, the malleus is visible as are air-fluid levels that can be seen in the anterior-inferior portion of the TM. The air-fluid levels indicate the middle-ear space (behind the TM) is being ventilated by the Eustachian tube.
Here is another example of a MEE.
Below is the complete video exam. Note the impressive ability of the Wispr digital otoscope to navigate past significant cerumen without requiring cerumen removal.

Mastoiditis
A 3-year-old male presents to the emergency department with ear pain. The parents report their son has had fever for “at least a week” with temperatures up to 104 F. He was seen in Urgent Care at the onset of his febrile illness where he was diagnosed with acute otitis media and started on an antibiotic. Upon physical exam the child has a temperature of 102.5 and mild nasal congestion without purulent drainage. He is very tender to palpation in the area posterior to his left ear where there is also distinct erythema and warmth of the skin. The external ear appears normal and his Wispr exam is below. The remainder of his exam is non-focal for a source of his fever.
Which of the following is true regarding the child’s condition?
- Continue the antibiotic prescribed by urgent care.
- It is the most common serious complication of acute otitis media (AOM).
- This condition is seen more frequently in adults than children.
- A CT scan is usually needed to guide treatment.
2. It is the most common serious complication of acute otitis media (AOM).
This child has acute otitis media (AOM) in his left ear and is presenting with signs and symptoms consistent with acute mastoiditis (AM), the most common complication of middle ear infections. While rare, affecting approximately 0.25% of AOM cases, the incidence of AM has increased over the past two decades likely attributable to increasing antibiotic resistance. The child’s continued AOM despite recent treatment with an appropriate course of antibiotics is suggestive of the presence of a resistant organism.
Young children, particularly less than 3 years of age, are more prone to developing AM due to immunologic, epidemiologic, and anatomic features unique to pediatrics. Anatomic factors including greater pneumatization of the mastoid bone as well as a smaller aditus ad antrum (the opening between the middle ear and the mastoid space) appear to play a central role. AOM leads to edema and debris blocking the aditus ad antrum, preventing the purulent drainage from exiting the mastoid air cells. If not treated properly this “otomastoiditis” may then progress to boney destruction and osteomyelitis formation as well as an array of other described complications including boney (subperiosteal abscess), vascular (internal jugular thrombosis), neurologic (facial nerve palsy), or intracranial (epidural abscess or sinus thrombosis) locations.
Younger age appears to be a risk factor for these complications and accentuates the importance of a thorough history and physical exam, even with the occasionally mundane complaint of “ear pain”. This is especially true since the signs and symptoms of uncomplicated AM generally do not differ from those of AOM. Suspicion is raised by persistent fever and more severe complaints or tenderness, erythema, and swelling in the poster auricular area—signs that may occur even in cases where there is still no complete erosion of the cortical bone or purulent collection. In more progressed cases, there may be anterior displacement of the auricle due to the evolving edema and associated cellulitis. Some experienced clinicians feel comfortable with diagnosing AM based on these physical findings, while many still rely on CT scans to evaluate for evidence of osteomyelitis or other any other complicating pathology noted above.
Management of AM includes initiation of IV antibiotics, typically a third-generation cephalosporin to extend coverage against resistant organisms. The placement of tympanostomy tubes may aid in resolution and allows culturing of middle ear fluid to guide further antibiotic therapy. Close monitoring in the hospital is required to assess the response to this therapy and anticipate additional surgical management for any indication of extension.
Here is the complete video exam:
Reference:
Pasquale Cassano, Giorgio Ciprandi, and Desiderio Passali. Acute mastoiditis in children. Acta Biomed, 2020; 91(Suppl 1): 54–59.

Visual Ear Diagnosis
A mother brings her 4-year-old daughter in for a well-child visit. A 4th-year medical student was assigned to do the history and physical. The mother has no concerns, but the child is clearly not happy to be at the clinic. The medical student presents the following image to you from the Wispr digital otoscope and is concerned that the left ear “looks infected.” What learning opportunity does this present for the student?
The child has prominent vasculature (erythema, redness), likely from crying.
This is a great learning opportunity for the student. The Wispr otoscope allows the learner to complete the exam independently and then review the findings with the attending on the built-in screen. In this case, there is increased redness due to dilated vasculature. This is often seen in the case of a crying or breath-holding child. If too brief and transitory a view of the eardrum is obtained, it’s easy to associate the “redness” with an infection that is not present.
WiscMed has assembled a visual ear diagnosis guide. The guide gives examples to the learner (and patients) of six common ear conditions seen in the primary clinic. The guide is available here as a web page or the guide is available here as a downloadable pdf.

Ear Canal Trauma
A 10-year-old previously healthy male presents to urgent care with concern for blood from his right ear. About an hour prior to presentation, he was playing in the woods. He believes a branch caught his ear. His Wispr digital otoscope exam is shown. What treatment is indicated?
The child has a mild abrasion to the posterior wall of his external ear canal. No treatment is necessary.

There is no evidence of active bleeding. The abrasion appears superficial. There is no foreign body present. From the video exam, it is clear that the tympanic membrane (TM, ear drum) is uninvolved. No topical or systemic antibiotics are indicated in this healthy child. Return instructions would include worsening pain, fever, changes in hearing, or bleeding.
Here is the complete video exam that demonstrates an intact ear drum:

Otitis Media with Effusion (OME)
A 37-year-old woman returned from Hawaii complaining of right ear discomfort. While she was in Hawaii, she had viral symptoms including a sore throat, mild fever, cough, and fatigue. She then developed right ear pain. She was seen at an urgent care clinic on the island and diagnosed with “an infection” along with an ear perforation and placed on an oral antibiotic and a topical ear antibiotic. Upon return to the mainland, the following image of her right ear was obtained with the Wispr digital otoscope.
What is your diagnosis and proposed treatment at this point?
The patient has otitis media with effusion (OME). There is no perforation present. Antibiotics are not indicated solely for this condition.
One of the key advantages of digital otoscopy is the ability to carefully review exam findings “on the screen” after the exam has been completed. In this case, the key clinical feature is the air-fluid level associated with OME. In addition, there is no bulging of the eardrum and the malleus is easily distinguishable. This rules out acute otitis media (AOM). There is no evidence of an eardrum perforation. The air-fluid levels indicate the Eustachian tube is functioning.

A middle ear effusion is fluid in the middle ear space, usually from inflammation secondary to a viral infection. The middle ear space is directly behind the ear drum. It’s partially visible to us because the eardrum is semi-transparent. After the initial exam, the patient was asked to perform the Valsalva maneuver. The Valsalva maneuver is pressure breath holding, familiar to us as we use the maneuver to “pop” our ears in a descending airplane. Here is the video of the patient performing the Valsalva maneuver. Note how obvious the air-fluid levels become as the increased air pressure in the middle ear moves the fluid about.
And here is the post-Valsalva image where the air-fluid levels are more distinct:
An interesting conclusion to this case is that when the presence of an OME is uncertain, having a cooperative patient perform the Valsalva maneuver may clarify the condition.

Resolving Acute Otitis Media
A 16-month-old female presents to the Emergency Department for evaluation of diarrhea and fever. She had been seen in Urgent Care the day prior and diagnosed with a viral illness and otitis media. The parents were instructed on supportive measures and a prescription for antibiotics was provided. Due to worsening diarrhea and concern for dehydration, she was brought in for re-evaluation. Her past medical history is significant for a completed course of antibiotics two weeks ago for an ear infection. She has otherwise demonstrated normal growth and development. In the emergency department, she is an afebrile, well-appearing toddler. She has a mild diaper rash. Her Wispr digital otoscope exam is shown.
How would you instruct the parents?
- Continue the course of antibiotics prescribed yesterday.
- Switch antibiotics.
- Consult to ENT
- Hold the prescribed antibiotic and provide continued supportive measures
4. Hold the prescribed antibiotic and provide continued supportive measures
The importance of good ear drum visualization for diagnosis is clear in this case. A 16-month-old child can be a particularly challenging exam. The features of the Wispr otoscope, particularly the thin speculum, increase the chances of successful imaging such as in this case.

The child’s Wispr exam does not demonstrate any of the hallmarks of active acute otitis media (AOM) to support the need for antibiotics. Specifically, she does not demonstrate moderate to severe bulging, mild bulging with concomitant intense erythema or bullae. However, her tympanic membrane does show evidence of a recent acute otitis media (AOM). First, there is a bulging of the pars flaccida portion of the tympanic membrane (TM). Second, she has several whitish spots consistent with dried purulence, “mud spots,” adherent to the middle ear surface of the TM, likely from a prior AOM. These findings (not to mention the gastrointestinal side effects of antibiotics) support the recommendation to hold the antibiotics, apply barrier ointment for the diaper rash, and encourage supportive measures for her likely viral gastroenteritis. Careful return instructions should also be provided.
Here is a Wispr University article that documents the resolution of AOM in daily images. Note that mud spots develop around day 9 of resolving acute otitis media.

Seed in Ear
A healthy 12-year-old who owns a pet parakeet arrives with concern for a foreign body sensation in his ear. He has no other complaints. The image is obtained with the WiscMed Wispr digital otoscope.
What is your diagnosis and treatment?
The patient has a bird seed in his external ear canal.
The patient’s pet parakeet was on his shoulder feeding. The bird decided it would be a good idea to store some seed for a rainy day. The external ear canal of the patient provided a convenient location.
Common foreign bodies in ear canals include ants, spiders, beads, hearing aid tips, earrings, tic-tacs, and pencil tips.
Removal of foreign bodies from the external ear canal can be challenging. More so in very young patients than in a cooperative 12-year-old. In this case, the nursing staff uneventfully removed the seed with water flushing. Other techniques for foreign body removal include the Katz extractor, forceps, suction, and “gluey surfaces.” In all cases, clear visualization and localization of the foreign body with the Wispr otoscope is helpful.
WiscMed thanks Dr. Daniel Lapidus of Pediatric Affiliates for this interesting case.
Here is the complete video exam:
Complete exam video

Myringoplasty
A three-year-old child presents to the emergency department (ED) with vomiting and diarrhea. She had recently been seen in the pediatric clinic following a procedure to remove her ear tubes. The child is afebrile with normal age-appropriate vital signs. She is well-appearing.
What abnormality is present in her Wispr otoscope ear exam?
There is a patch (myringoplasty, MP) to the anterior inferior tympanic membrane (TM, ear drum).
Additional medical history for our patient included recurrent acute otitis media (AOM) throughout her first year of life resulting in tympanostomy tube (ear tube, ventilation tube) placement. The child had done very well with fewer episodes of otitis media, however, at her three-year well-child visit it was noted her left tube was still in place. Therefore, she underwent removal and paper patch myringoplasty (MP, see arrow below). Today’s exam shows the well-positioned patch. In addition, the malleus bone is discernable, and the tympanic membrane (TM, ear drum) is normal suggesting a properly healing repair without evidence of infection.

Tubes are placed in the anterior inferior quadrant of the ear drum. They typically fall out on their own in 6 to 18 months with removal being recommended if the tubes are present after two to three years. For spontaneously extruded tubes, persistent TM perforation occurs in 2% of patients with short-term tubes and 16% with long-term tubes. However, in children requiring surgical tube removal, persistent TM perforation is generally anticipated and myringoplasty via insertion of paper (such as in our patient), steri-strips, gel foam, or a collagen matrix patch is performed to encourage closure. While the reported success rates for myringoplasty techniques vary, a recent meta-analysis suggests no difference in perforation closure between patching versus no patching, regardless of the material used by the surgeon. In another study, 13% of children undergoing this procedure still had persistent perforation. Factors influencing persistent perforation included patient age, number of tubes previously placed, perforation size, and presence of myringosclerosis.
Here is an example of a healed myringoplasty.
The patient’s presenting symptoms of vomiting and diarrhea were felt to be secondary to gastroenteritis, unrelated to her myringoplasty. After an oral dose of anti-nausea medication and a successful oral fluid challenge, she was discharged home with supportive measures. No further action about her myringoplasty was necessary at today’s encounter.
Here is the complete video from the exam.
Complete exam video
Michel M, Nahas G, Preciado D. Retained Tympanostomy Tubes: Who, What, When, Why, and How to Treat. Ear Nose Throat J. 2020 Aug 31.
Tan GX, Hamilton A, MacArthur C. A Systemic Review and Meta-Analysis: Timing of Elective Removal of Tympanostomy Tubes. Laryngoscope. 2022;132(10).
Brown C, Behar P. Factors affecting persistent tympanic membrane perforation after tympanostomy tube removal in children. Int J Pediatr Otorhinololaryngol. 2020 Mar;130.

Ventilation Tube
A 6-year-old male presents to the pediatric clinic for a well-child visit. The parents have no concerns for today’s visit. They note that he has a history of recurrent ear infections and had “ear tubes” placed 3 months ago. They ask for your evaluation of the tubes. His right ear exam from the WiscMed Wispr otoscope is shown.
What is your advice to the parents?
The ventilation tube is properly positioned, patient and the eardrum is normal. No action is necessary.

Ventilation tubes, also called tympanostomy tubes or ear tubes are often placed when a child experiences recurrent acute otitis media (AOM, “ear infection”). The tube is just like it sounds, a hollow cylinder that is placed through the ear drum. In this image, you can see the “backside” of the ventilation tube through the semi-transparent eardrum. The tubes purpose is to drain inflammatory fluid from the middle ear space and to equalize pressure on both sides of the eardrum. Normally, the pressure in the middle ear space is equalized by the Eustachian tube. The Eustachian tube is a hollow, noodle-like structure that connects the middle ear space to the posterior nasal pharynx (roughly the back of the mouth). When inflamed, the Eustachian tube becomes blocked, and it is no longer able to equalize pressure in the middle ear space. This causes painful bulging of the ear drum as seen in the example of acute otitis media below.
 Acute Otitis Media (AOM) Example
Acute Otitis Media (AOM) Example
In recurrent cases of infection, ventilation tubes are placed to mimic the function of the Eustachian tube. They are commonly placed in the anterior inferior quadrant of the tympanic membrane. The tube drains inflammation in the middle ear space and relieves the painful middle ear pressure. Almost everyone has experienced mild middle ear pressure when an airplane descends. We unconsciously know to increase the pressure in our mouth which expands the Eustachian tube and “pops” our ears, thus equalizing the pressure on both sides of the eardrum. This is technically known as the Valsalva maneuver.
In this case, the ventilation tube appears to be patent. There is no bulging of the ear drum. The malleus bony landmark is clearly visible. There is no erythema. The child reports no discomfort. All these items suggest a normal eardrum aside from the presence of the therapeutic ventilation tube.
Ventilation tubes typically fall out on their own in 6 to 12 months.

Middle Ear Effusion
A 30-month-old boy presents to the emergency department (ED) with a chief complaint of fever and cough for six days. His mother states her child was seen two days ago in Urgent Care and was negative for influenza, RSV, and Covid. He was diagnosed with bilateral otitis media and started on amoxicillin. Despite receiving three doses so far, he again had a fever last night to 102 F as well as a harsh cough. Mom brought him into the ED wondering if he needs to be on a different antibiotic. The child is afebrile and well-appearing. His voice is slightly hoarse, but his cough is neither barky nor productive. His Wispr otoscope exam is shown here. Should the child be switched to a different antibiotic?
No, the infection is resolving as expected. No change in treatment is indicated.
This child presents with concerns that symptoms have not fully resolved despite being on antibiotics for bilateral acute otitis media (AOM). This is a common scenario, one that raises the question of what constitutes treatment failure after initiating antibiotics for AOM.
It is generally felt that it takes 1-2 days for antibiotics to begin decreasing middle ear bacterial burden and tympanic membrane (TM) inflammation. Additionally, most children with AOM will demonstrate improvement in symptoms within 2-3 days. Given this timeframe, one might consider treatment failure if the child is continuing to have significant symptoms and the TM continues to appear bulging on exam beyond 3 days. That is not the situation for this patient.
The child in this case has a middle ear effusion (air-fluid levels in the middle ear) and mild bulging in the superior portion (pars flaccida) of the TM. This suggests that the Eustachian tube is properly venting the middle ear space. He does not have intense erythema and his mom does not endorse significant pain. Furthermore, the overall appearance of the TM is reassuring—it is translucent and there is a light reflex. These signs were discussed with the parent who felt reassured that the AOM was appropriately resolving, and the parent was instructed to continue with current management. Careful return instructions were given.
The development of AOM in images and its resolution are documented in this Wispr University article.

Hemorrhagic Bullae
A first year Pediatric resident presents the case of a 7-year-old female brought to the emergency department (ED) with a chief complaint of ear pain. According to the child’s parents, the ear pain worsened to the point of waking the child. She was diagnosed with influenza earlier in the week but seemed to be doing better with only a mild cough. Her fevers had continued and were responsive to ibuprofen.
The child’s physical exam is unremarkable except for her left tympanic membrane (TM) which the resident displays on the Wispr otoscope for review. The resident summarizes her assessment of the patient as “I believe she has acute otitis media but I’m struggling to describe the findings.”
Does this child have acute otitis media (AOM)?
Yes, the child has AOM.
The resident can be forgiven for some uncertainty in describing his patient’s TM findings as there seems to be a lot going on and demonstrates why it is helpful to take a stepwise approach to our assessments. As described in Seeing is Believing Part 2, to determine whether a child has acute otitis media (AOM), begin with identifying the presence (or absence) of bulging. A few questions can help with this:
Does the TM look like a bagel/donut?
-If yes, then there is likely to be at least moderate bulging of the TM and a high likelihood of acute otitis media.
-If no, then we need to look at other landmarks and ask additional questions:
Can you clearly see the malleus?
-If yes, then the TM is not bulging and the likelihood of AOM is low.
–If no, then there is likely bulging in the pars flaccida (i.e. upper portion) of the TM, indicating at least mild bulging or “fullness” of the TM. This is not sufficient to diagnose AOM, so we need to ask an additional question:
Is there intense erythema of the TM? -or- Is the child demonstrating significant ear pain?
–If yes to either question, then there is a high likelihood of AOM.
–If no to either question, then then the likelihood of AOM is lower and antibiotics are not indicated.

When posed with these questions, the resident responded with: “No, the TM does not look like a donut. No, I cannot make out the malleus. Yes, the child’s TM has intense erythema and a lot of ear pain. I feel confident in the diagnosis of AOM.” Following this exchange, further bedside teaching allowed a more detailed level of analysis. The child’s TM appears to be developing a bullae consistent with bullous myringitis inferiorly and has a hemorrhagic bullae centrally. The resident endorsed being initially confused by these findings but reported a much greater degree of certainty in his ability to walk through the steps to accurately diagnose AOM. This is an advantage of the digital otoscopy that the Wispr provides.
Here is the complete video exam.
Complete exam video
Lieberthal A, Carroll E, Chonmaitree T et al. The Diagnosis and Management of Acute Otitis Media. Pediatric, Mar 2013; 131(3).
Rothman R, Owens T, Simel D. Does this Child Have Acute Otitis Media? JAMA, Sept 2003; 290(12):1633-1640.

Normal Ear
A 15-year-old female presents to the pediatric clinic for a routine sports exam. She is well and has no complaints. This image of her right ear is obtained. She is a curious student and asks you to identify and explain the structures seen in the image.
What structures would you choose to identify and explain?
One of the benefits of youth is that anatomy is often pristine, as in the case of this beautiful right ear image.
The ear drum (tympanic membrane, TM), separates the outer ear from the middle ear space. It is the only structure that is “outside.” The other features are “behind” the translucent eardrum in the middle ear space. Think of the eardrum as being a cloudy layer of taught saran wrap. The surface responds to sound waves by vibrating. This vibration must be turned into a signal that our brain can process.
The job of translating the vibration to the inner ear is accomplished by a chain of three tiny bones; the malleus, incus, and stapes. These are often referred to as the hammer, anvil, and stirrup. The malleus is directly attached to the inner surface of the eardrum. As the eardrum vibrates, the malleus moves with the vibration. The malleus is connected to the incus and the incus to the stapes. Through these connections, the tiny movement of the eardrum is mechanically amplified and delivered to the inner ear. In the inner ear (not visible), this movement is converted to a fluid action that moves tiny hairs which create the nerve signal to the brain. It’s a beautifully engineered system.
Also visible in this image is the chorda tympani nerve. It runs behind the malleus and in front of the incus. This nerve has nothing to do with the ear, it simply borrows the middle ear space to get “where it needs to go.” It provides taste sensation from part of the tongue along with secretory signals. It’s unusual to be able to see this nerve so clearly.

Otitis Media with Effusion
A 3-year-old presents to the pediatric emergency department (ED) with a chief complaint of wheezing. She has had several days of nasal congestion and was seen in an urgent care the prior evening where she was diagnosed with acute otitis media (AOM) and started on amoxicillin. The evening of presentation she was having shortness of breath. Her parents brought her in for evaluation. On physical exam, she is afebrile with a RR 40, HR 156, and Pox 96% on room air. She has mild course breath sounds bilaterally but no wheezing or increased work of breathing.
Her Wispr exam is notable for this image.
True or False:
This child should continue her amoxicillin.
False. The child has otitis media with effusion (OME). Antibiotics are not indicated.
Discussion:
This child’s Wispr exam demonstrates a mildly retracted tympanic membrane (TM) as evidenced by the slightly prominent malleus and a smaller, displaced light reflex. An additional finding is the presence of a yellowish/amber effusion inferiorly, thus her diagnosis is consistent with otitis media with effusion (OME). OME may be present in the setting of a resolving acute otitis media (AOM) or eustachian tube obstruction (i.e. an upper respiratory infection in a child) without infection, therefore antibiotics are not warranted.
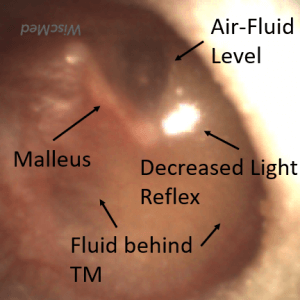
Various changes including air-fluid levels behind the TM, amber or gray color, displacement of the light reflex, mild to severe retraction, and accentuated landmarks are hallmarks of OME. This is in contrast to AOM in which mild to moderate bulging is the most sensitive indicator of bacterial infection. It is worth repeating that visualization of the tympanic membrane is critical to differentiate between AOM and OME and prevent the unnecessary prescription of antibiotics. The child in this case was discharged home with supportive measures for her respiratory illness and the recommendation to discontinue antibiotics. Most cases of OME resolve spontaneously in two to four weeks. Follow-up with a family physician is recommended if parents have ongoing concerns.

Neonatal Acute Otitis Media
A 6-week-old male infant presents to the Emergency Department (ED) for congestion and fussiness. He was born at full term without complications and had been doing very well despite a recent onset of cough. However, earlier that evening he developed a fever to 101.5, and, after calling their pediatrician’s nursing line, the family was directed to the ED for evaluation. Upon arrival, the child had a temperature of 101.2 F, RR 52, HR 160, and POx 96% on room air.
He was well-appearing with very mild retractions and occasional wheezes. His Wispr exam is shown here. The remainder of his examination was non-focal. The infant received a dose of acetaminophen and nasal suctioning which improved his work of breathing and decreased his RR to 45. A respiratory panel was collected which resulted positive for the respiratory syncytial virus (RSV). His urinalysis was negative (culture sent) and a complete blood count (CBC) demonstrated a white blood count of 6,000 with less than 5% bands.
What is your diagnosis and treatment?
The infant has laboratory-proven RSV with clinical evidence of acute otitis media (AOM).

The infant in this case has a clear case of RSV bronchiolitis, a condition that has spread across the pediatric landscape like wildfire in the fall of 2022. In addition to his respiratory illness, the infant also has strong evidence of acute otitis media (AOM) with moderate bulging, loss of landmarks, and a purulent effusion noted on his Wispr exam. The association between RSV bronchiolitis and AOM is well-described (1-3), so perhaps it is not surprising there has also been a significant jump in the diagnosis this season—one that may be contributing to amoxicillin shortages seen in certain parts of the country (4). The causative pathogens in infants are felt to be the same as in older children, however many clinicians rightfully exercise caution with diagnosing AOM in the very young infant out of fear of missing a serious bacterial illness (SBI) (5,6).
In his 2018 Pediatric EM Morsels article, Dr. Sean Fox provides an eloquent and succinct discussion of the pitfalls associated with neonatal AOM (5,6). Major challenges include 1. Adequately visualizing and appreciating the anatomic uniqueness of the TM in infants, and 2. Should AOM be considered an SBI requiring septic work-up in infants? While no gold standard for evaluation exists, interpretation of the available evidence suggests following the typical risk stratification for infants older than 28 days—usually including CBC, urinalysis, and (when appropriate) respiratory viral swabs. For the well-appearing infant with low-risk stratification, management with an oral antibiotic and close follow-up is reasonable. However, for neonates less than 28 days of age with fever, this approach may not be advisable as it is unclear if AOM remains localized in this very immature cohort (6). The patient in our case was started on high-dose amoxicillin and at follow-up appeared to be doing very well and was no longer febrile.
Prior to this case, the author (with over 20 years of pediatric ear exams), had never confidently observed AOM in such a young child. Similar to the experience described in Dr. Fox’s discussion, I will admit to being slightly dubious when I am told that a neonate has been diagnosed with AOM. However, as observed in this case, digital otoscopy has once again helped address the major challenge of visualizing the TM, provided much greater diagnostic certainty, and may offer a tool for future research on AOM in this very young cohort.
Here is the complete video of the exam:
Complete exam video
References
1. Risk of acute otitis media in relation to acute bronchiolitis in children
Gomaa MA, Galal O, Mahmoud MS.Int J Pediatr Otorhinolaryngol. 2012 Jan;76(1):49-51.
2. Acuteotitismedia in children with bronchiolitis
Andrade MA, Hoberman A, Glustein J, Paradise JL, Wald ER.Pediatrics. 1998 Apr;101(4 Pt 1):617-9.
3. The clinical course of bronchiolitis associated with acute otitis media
Shazberg G, Revel-Vilk S, Shoseyov D, Ben-Ami A, Klar A, Hurvitz H.Arch Dis Child. 2000 Oct;83(4):317-9.
4. https://www.livescience.com/amoxicillin-shortage-explained
5. https://pedemmorsels.com/neonatal-acute-otitis-media/
Sakran W, Makary H, Colodner R, Ashkenazi D, Rakover Y, Halevy R, Koren A.Int J Pediatr Otorhinolaryngol. 2006 Apr;70(4):613-7

Bullous Myringitis
A 4-year-old male is brought to the Pediatric emergency department (ED) at 1 am for a complaint of severe ear pain. He was in such discomfort that his mother was concerned he had poked himself in the ear before bedtime while “aggressively” cleaning his ears with a Q-tip. However, she denies seeing any blood and he has been otherwise well without fever or congestion. A physical exam revealed an uncomfortable child holding his hand over his right ear.
The Wispr exam is shown below.
What is your diagnosis, and how could the pain be managed quickly?
The child has bullous myringitis. Topical analgesics will help reduce the pain.
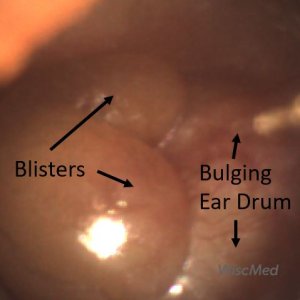
It is understandable why this child is so miserable as he has severe bullous myringitis. This is often considered to be on the spectrum of acute otitis media. The two large blisters and tympanic membrane bulging make identification of any middle ear landmarks impossible. The severity of this case is unusual, but the initial management is not. Alcaine (proparacaine) drops were instilled into the ear and a dose of oxycodone was provided in the ED. Within 20 minutes the child reported significant relief and was discharged home on scheduled ibuprofen and a course of antibiotics (see this case for a discussion of usual pathogens). Due to the severe degree of his case, it was also recommended he follow up closely for resolution of the inflammation and audiology if any hearing concerns.
Several studies have previously demonstrated the beneficial effect of topical anesthetic in treating the pain associated with otitis media, most recently a 2008 study in the Journal of Family Practice investigated the use of 2% lidocaine (which is readily available in EDs as the IV formulation) as a topical anesthetic instilled into the ear canals of children presenting with AOM. J Fam Pract. 2008 Jun; 57(6): 370–373.
Here is the complete video exam:
Complete exam video

Otitis Externa
A previously healthy 13-year-old female presents to the pediatric clinic with concern about ear pain. She has been on summer break and spending time swimming in the local lake. The pain began to develop in her right ear about 2 days ago and has steadily gotten worse. She reports that hearing seems “strange” in that ear and that there has been a yellow discharge. The ear is “itchy.” She has not had any fevers or headaches. Over-the-counter analgesics have been only modestly helpful with the pain. She does not have any prior history of ear infections. This image of her ear is obtained with the Wispr digital otoscope.
What is true about this condition?
- It occurs from prolonged exposure to cold water.
- It is associated with trauma to the ear canal.
- Eustachian tube dysfunction is a risk factor.
- It’s most common in adults over 20 years of age.
The answer is 2. It is associated with trauma to the ear canal.

The patient has otitis externa, or an infection of the external ear canal. It is commonly known as “swimmer’s ear.” The eardrum is not visible due to the purulence occluding the canal. Otitis Externa is commonly seen in swimmers in the 5 – 14 year age group. It’s caused by a breakdown in the protective layers of the ear canal. Trauma such as from q-tips or ear pods or retained foreign bodies are common sources of micro-trauma that irritate the canal, remove the cerumen (wax) barrier, and allow bacteria from water sources to cause the infection. Warm summer swimming is a common part of the history of a patient with otitis externa. The infection is in the external ear canal and not associated with the middle ear, therefore the Eustachian tube is not involved. Prolonged exposure to cold water is a risk factor for exostosis, known as “surfer’s ear.”
Compare acute otitis media (infection in the middle ear space, “behind the ear drum”) to otitis externa (infection of the external ear canal, “in front of the ear drum”).
Treatment for a moderate case of otitis externa such as this one would be a topical antibiotic with a steroid. A wick is often used to assure that the medication is delivered to the entire external ear canal. Careful return instructions should be given in the case of worsening pain or fever.

Diffuse Sclerosis
A 35-year-old woman stopped by the WiscMed booth at the 2022 American Academy of Pediatrics (AAP) tradeshow. She told WiscMed staff that she had “interesting ears.” She had a history of many years of significant allergies that she attributed to her ear changes. She does not have any ear pain, nor does she have any hearing loss. The following image of her right ear is obtained with the Wispr digital otoscope.
What change to her ear drum is notable?
The woman has diffuse sclerosis of her eardrum.

Sclerosis of the tympanic membrane is caused by changes to the submucosa of the middle ear. Thought to be a cellular response to insult, the “whitish” appearance is associated with calcium deposits. Hearing is generally not affected. Sclerosis is usually caused by infection or by trauma, the trauma is often the result of the placement of ventilation tubes. In the case of sclerosis secondary to ventilation tubes, the pattern is often localized. In this case, given the history report of the patient, it’s possible that diffuse sclerosis represents a more generalized immune response to recurrent allergic episodes.
Compare diffuse sclerosis to localized sclerosis to normal.
Here is the complete video exam:
Complete exam video

Bleeding Ear Canal
A 25-year-old pediatric resident stopped by the WiscMed booth at the American Association of Pediatrics. She experienced bleeding from her left ear canal two weeks ago. She does not report any trauma to the ear. The bleeding was minor and lasted only a short time. This image was obtained of her left ear.
What are possible explanations for the reported bleeding?

The image shows a healthy and normal tympanic membrane (TM, ear drum) and malleus with an apparent anomaly on the posterior-superior portion of the ear canal. If the resident had not reported a remote episode of bleeding, this could be assumed to be cerumen (ear wax). Given the report of past ear canal bleeding, this area most likely represents dried blood, possibly from a minor scratch. Since the resident was clear that there had been no trauma to the ear canal, the source is a matter of speculation. Possible causes include unrealized trauma from a Q-tip, an insect bite, or less likely a superficial vascular anomaly that is prone to injury. Follow-up would only be necessary if there is a repeat of significant bleeding.
Here is the complete video of the exam:
Complete exam video

Shagrination or “Cobble Stoning”
A four-year-old female is brought in to the pediatric clinic for re-evaluation. Two days ago she was seen for fever and ear pain. She was diagnosed with acute otitis media and placed on antibiotics. The mother reports that the child is feeling much better. The fever and ear pain have resolved and she is once agina playing with her normal abandon. The following image of her ear was obtained. What is true about this condition?
- A different antibiotic needs to be considered.
- ENT should be consulted.
- Tympanostomy tubes would prevent this in the future.
- The child’s infection is resolving as expected.
The answer is 4. The child’s infection is resolving as expected.
This patient has the classic appearance of shagrination or “cobble stoning” of the tympanic membrane (TM).

The roughened appearance, shagrination (cobble stoning) of the TM is thought to occur during the course of acute otitis media (AOM) as the bulging membrane begins to return to its normal position as fluid in the middle ear recedes. While the exact pathophysiology is not clear, this finding reminds us that the TM is not a single homogeneous band of tissue but rather a multi-layered complex composed of epithelial (continuous with the external canal), fibrous (middle radial layer), and mucosal (continuous with the lining of the middle ear) cells.
Armengol and Handley published images of 17 children with AOM who either developed or presented with shagrination1. Follow-up images indicated that resolution of bulging typically occurred within 1-2 days, suggesting that shagrination indicates the decompression of the middle ear space (think of the wrinkles in a deflated balloon or stretch marks) with a resolution likely to occur soon thereafter.
The images below suggest the path to resolution from acute otitis media (AOM). As the AOM infection resolves, the bulging begins to “deflate” causing the shagrination. Complete resolution of the infection returns the tympanic membrane to its normal condition.
As can be attested by many of the Wispr cases, the use of digital otoscopy facilitates not only the diagnosis of AOM but also provides opportunities to evaluate the significance of physical findings. In the Armengol paper, digital otoscopy demonstrated resolution of AOM findings within 1 to 2 days following the appearance of cobblestoning, including in three patients who did not receive antibiotics. While further studies in a larger cohort will be helpful, this suggests that the appearance of shagrination may herald spontaneous resolution and allow antibiotics to be avoided or curtailed in these patients. For further information, here is a case study of resolving AOM. In this study, shagrination appears on day 8.
Here is the complete video of the exam:
Complete exam video
- Armengol, CE, and Hendley, JO, “Shagrination during Acute Otitis Media,” The Journal of Pediatrics, 2014;165:870.

Middle Ear Effusion
A 12-year-old female presents to the pediatric clinic for a routine well-child appointment. The patient reports that a few days ago she had a cough, runny nose, and congestion. Today, she says the symptoms have resolved and she feels well.
This image of the right ear was obtained.
What is true about this condition?
- It is caused by a blockage in the Eustachian tube.
- The source is bacterial.
- Tympanostomy (ear) tubes are indicated.
- No intervention is needed.
The answer is 4. No intervention is needed.
The child has a middle ear effusion.
This is a common clinical scenario, an incidental finding on a physical exam. The ear is not normal in that there is fluid behind the tympanic membrane (eardrum). This is referred to as a middle ear effusion.

The presence of air-fluid levels suggests both inflammation of the middle ear space and proper ventilation. The inflammation is no doubt due to sequala of the minor viral syndrome the patient has described recovering from. The air-fluid levels let us know that the middle ear space is being properly ventilated by the Eustachian tube. There is a mild bulging of the pars flaccida portion of the TM. This is the ”loose” portion of the TM and responds to even a small increase in middle ear pressure. The important finding is that the TM is not bulging, and the malleus bony landmark is clearly identifiable.
Contrast the middle ear effusion with acute otitis media (AOM) below. Not the marked bulging across the entire TM in the case of AOM. There are also no air-fluid levels in AOM which means the middle ear space pressure is not being equalized via the Eustachian tube.
Middle ear effusions typically resolve in days to weeks. No treatment is generally needed. Here are two other examples of middle ear effusions – one, two.

Bullous Myringitis
A 6-year-old male presents to the emergency department (ED) late in the evening with a complaint of left ear pain for the past hour. The child had been fighting an upper respiratory infection (URI) with congestion and low-grade fever for the past several days but had otherwise been well. The physical exam is remarkable for a crying child holding his hand over his left ear. He has moderate rhinorrhea.
His Wispr exam is notable for this image.
Which of the following is true regarding the child’s condition?
- Peak incidence occurs in the summer months.
- Diagnosis may require laboratory studies.
- This is a painless condition.
- Treatment should include consideration of antibiotics.
Answer: 4, Treatment should include consideration of antibiotics.
The child has bullous myringitis (BM), a relatively common infectious condition characterized by blisters (bullae) on the tympanic membrane (TM). BM may be on the “more severe” end of acute otitis media (AOM). It has the features of acute otitis media, bulging, loss of bony landmarks, and erythema (redness) with the additional finding of blistering on the TM.

Bullous myringitis has a peak incidence during the winter months corresponding to the traditional peak in respiratory viruses that play role in its pathogenesis. Among younger children, respiratory viruses including RSV and influenza predominate. Streptococcus pneumoniae is the most identified bacteria and is found in a higher prevalence in bullous myringitis compared to AOM. No further laboratory studies are needed to make the diagnosis. In the primary clinical environment, it is a visual diagnosis.
Bullous myringitis is often more painful than the typical case of AOM and clinicians should consider more aggressive management, including the use of topical anesthetic such as viscous lidocaine. The American Association of Pediatrics (AAP) recommends oral antibiotic regimens as appropriate. A follow-up to assess for resolution and any evidence of hearing loss is prudent as studies have observed a higher risk of recurrent AOM as well as hearing deficits following bullous myringitis.
Here is the complete video of the exam:
Complete exam video

Bilateral Acute Otitis Media (AOM)
A six-year-old female is brought into the pediatric clinic for evaluation of ear pain. Four days ago, the child began to have cough, rhinorrhea, and throat pain. Two days ago she was evaluated at urgent care where a rapid strep was negative and she was diagnosed with a viral infection. Since that visit, the child continues to have a temperature to 39 C, now with bilateral ear pain. The parents have been treating the child with over-the-counter analgesics which temporarily help with the symptoms. The following image of her right ear was obtained with the Wispr digital otoscope.
What is your diagnosis and treatment?
The child has acute otitis media and antibiotics should be considered.
This is one of the most common reasons for a pediatric visit, a viral syndrome that may evolve into acute otitis media with ear pain. This patient has bilateral acute otitis media as the images below demonstrate.
What starts as an apparent viral infection can lead to obstruction of the Eustachian tubes. The Eustachian tubes vent the middle ear space to the posterior nasal pharynx. When this tube becomes blocked, it’s possible for a bacterial co-infection to take place. A consequence of the infection and blockage is the bulging of the tympanic membrane (ear drum) because the pressure on the “inside” of the ear is higher than the external air pressure. The other features of the infection are erythema (redness) and loss of the bony landmarks. The umbo dimple is often prominent and makes the entire eardrum look like an “angry donut.” It looks painful, and it is. Hearing is often diminished because the eardrum is not able to vibrate normally.

After initiation of antibiotics, the symptoms of AOM (pain, fever, hearing decrease) generally resolve quickly while the physical findings may take several weeks to return to normal as shown here.
Here is the complete video exam of both ears. Note the ability of the Wispr otoscope to navigate the small canals partially occluded by cerumen (wax).
Complete exam video

Fibrous disk
A 42-year-old male is seen by his primary physician for a routine checkup. He has no complaints. This image of his right ear is obtained.
What abnormalities do you appreciate and what interventions are indicated?
The patient has a fibrous disk along with pseudo retraction of the pars flaccida. No intervention is indicated.

This image shows the middle ear anatomy nicely. The malleus and incus ossicles are clearly visible. The chorda tympani nerve can also be identified although it is not labeled due to space constraints. This image has several features that distinguish it from a “normal” tympanic membrane. The most obvious is the large fibrous disk. The tympanic membrane (eardrum) is comprised of three layers of tissue. The (1) outer cutaneous layer, the (2) middle fibrous layer, and the (3) inner mucosal layer. In the case of this patient, it appears that there is a localized thickening of either the outer cutaneous or middle fibrous layers. The cause of this is not known, but it does not seem to involve either infection or trauma. It is likely of embryologic origin.
In addition to the fibrous disk, there is also pseudo retraction of the pars flaccida portion of the tympanic membrane. The tympanic membrane divides the external ear from the middle ear. The portion of the membrane that drapes across the superior portion of the malleus bone can become retracted for several reasons. One reason is a prior history of trauma or infections, the other is compressed geometry of the ear canal. In this case, the compressed geometry of the ear canal is likely causing a fold of the tympanic membrane. This might be considered a pseudo retraction. Compare with a pars flaccida retraction.
Neither the fibrous disk nor the pseudo pars flaccida retraction are concerning. They likely have no effect on hearing. No intervention is needed.

Erythema
A four-year-old previously well male is brought into the emergency department at 2 am by his parents with concern for cough. The daycare attending child has had 3 days of cough, runny nose, and mild fever. The parents report that multiple children at daycare have been ill recently. The child continues to eat and drink, but with less enthusiasm than typical for him. They have been treating his symptoms with over-the-counter medications. On exam, the child appears ill without being toxic. He has a temperature of 38 C, appropriately resists the exam, and is crying robustly. He has copious tears and oral secretions. The following image of his right ear is obtained.
What are your diagnosis and treatment?
The child’s ear is erythematous (red), but there is no sign of infection. He likely has a viral infection.
An advantage of the Wispr digital otoscope is the ability to capture images and videos. This allows you to review the image on the device without the pressure of making a diagnosis while examining a squirming child. If a practitioner only had a brief glimpse of this ear, it is likely that the impression would be of marked erythema (redness) without also recognizing that there are no other signs of infection such as bulging or loss of bony landmarks. It’s possible that the child could be inappropriately started on antibiotics with only a brief glance. The Wispr otoscope gives time for thoughtful review of the exam. Because there is no sign of infection, antibiotics are not indicated.

Note that in this case there is no bulging of the tympanic membrane (TM, eardrum) and that the malleus bone is clearly visible. There are several irregularities of the TM of unknown origin that may be effusions although that is not supported by the appearance of the rest of the TM. Compare this case to acute otitis media (ear infection) and normal.
The cause of the erythema is most likely crying.

Acute Otitis Media (AOM)
A 3-year-old female presents to urgent care with her parents for evaluation of fever and ear pain. The parents report that the child has had three days of viral symptoms including cough, runny nose, and a temperature to 38 C. They have been treating her with over-the-counter analgesics to which she has responded well. This morning the child began to complain of ear pain. She does not have any history of ear infections and has been well. The following image is obtained with the Wispr digital otoscope.
What is your diagnosis and treatment?
The child has acute otitis media (AOM) and antibiotics should be considered.
This is a very common presentation in acute care. A pediatric patient with a prodrome of viral symptoms advancing to ear pain. The Wispr digital otoscope image shows all the features of acute otitis media (AOM). There is bulging of the ear drum, loss of bony landmarks, and erythema (redness). The bulging is from increased pressure in the middle ear space because the Eustachian tube is not properly ventilating this area. A notable feature of the bulging is the dimple in the middle. This is caused by the distal portion of the malleus bone, the umbo. The result is painful distension of the tympanic membrane (TM, ear drum).

Compare this ear with AOM to a normal ear. It’s easy to tell the difference between the two ears, and also apparent why an ear infection is painful.
Treatment generally involves an oral antibiotic along with topical or systemic pain control. Although the child likely started with a viral infection, when it advances to AOM there is often bacterial co-infection, thus the indication for antibiotics. This Wispr University article tracks the development and resolution of an ear infection through daily images.
Here is another example of AOM.
Here is the complete video exam. Note the ability of the Wispr otoscope to navigate the small canal, bypass cerumen (wax) and obtain a diagnostic image.
Complete exam video

Developing Acute Otitis Media (AOM)
A 4-year-old female presents to the emergency department (ED) for evaluation of fever and ear pain. Her parents note she has had mild congestion for the past week but otherwise was well until that evening. Shortly after going to bed, the child woke with right ear pain. The parents gave her a dose of acetaminophen and put her back in bed. However, less than an hour later the child woke with worsening pain so she was brought in for concerns of an ear infection.
In the ED, the child is well-appearing and afebrile. There is mild congestion with clear rhinorrhea. The Wispr exam is shown here. Based on the AAP otitis media clinical practice guideline, how should this be managed?
The child likely has developing acute otitis media (AOM) and antibiotics should be considered.

This child’s ear exam demonstrates mild bulging, or “fullness”. The notable characteristics are the indistinct malleus (due to the bulging in the pars flaccida) superiorly and a shallow dimpling in the center of her tympanic membrane. Mild bulging can be caused by other conditions such as fever, crying, Eustachian tube dysfunction, and resolving otitis media. To help differentiate (likely early) acute otitis media demonstrating mild bulging from these other conditions, the 2013 AAP Clinical Practice Guideline on Diagnosis and Management of AOM recommends additional signs (intense erythema) and symptoms (pain) ought to be present. The presence of such additional findings increases the likelihood of AOM significantly.
The current patient demonstrates pain as well as injection of the tympanic membrane (TM). Given this clinical picture, one could reasonably elect to treat with antibiotics. In this child, we elected to treat her pain with topical anesthetic and provide a prescription to be filled the following day if the pain persisted. The rationale for this approach is that we felt managing the child’s late-night pain was more important than immediate initiation of antibiotics. Also, while there is certainly prominence of the vasculature to her TM, we did not feel this raised to the level of “distinct erythema” referenced in the AAP guideline. Thus, we also felt waiting a short period to see if symptoms more strongly indicated an evolving AOM was appropriate.
Upon follow-up call the following evening, the family reportedly filled their prescription shortly before dinnertime.
Here is the complete video exam:
Complete exam video

Myringosclerosis
A 17-year-old male presents to the pediatric clinic for a routine sports exam. He has no complaints. He has a history of a tympanic membrane perforation of his right ear. Examination of his right ear with the Wispr digital otoscope reveals this image.
What is your diagnosis?
The patient has myringosclerosis (sclerosis) with evidence of a healed perforation.
The tympanic membrane (ear drum) is made up of three relatively thin layers of tissue. This allows the eardrum to vibrate from sound waves, but it also makes the structure susceptible to perforations. A perforation can occur from high-intensity sound waves like a firecracker, from pressure in diving into the water, or from devices such as q-tips or earbuds. A perforation can also be caused “on purpose” by a medical procedure to install ear tubes.

When the perforation heals, there is often evidence of sclerosis as seen in this case. Sclerosis is seen as “white patches” on the ear drum. It can often be quite extensive. Generally, there are no consequences to hearing. The area of sclerosis can change with time as the tympanic membrane is constantly evolving.
Here is the complete video exam:
Complete exam video

Tympanostomy or Ventilation Tubes
A 4-year-old male returns to the pediatric clinic for a follow-up evaluation. Six months ago the child had ear tubes (tympanostomy or ventilation tubes) placed by ENT for recurrent acute otitis media. The mother reports that the child has been doing well. She has no concerns for her child today. The following image is obtained by the Wispr digital otoscope during the visit.
What should the mother be told about the ear tubes?
The child has a ventilation tube that appears to be partially extruded.
Ear tubes have several medical names. They are commonly referred to as tympanostomy or ventilation tubes. All three names, ear, ventilation, and tympanostomy refer to the same thing, the placement of a tube through the eardrum to drain fluid from the middle ear space and to equalize pressure on both sides of the eardrum. Normally, the Eustachian tube provides this drainage and equalization of pressure function. The Eustachian tube is a “floppy noodle-like” tube that extends from the middle ear space to the posterior nasal pharynx. This tube can become blocked by inflammation and infection leading to increased fluid and pressure in the middle ear. This is painful and causes a bulging ear drum. In children that have recurrent problems with Eustachian tube dysfunction, a ventilation tube like this one may be placed in the eardrum. This drains the fluid and equalizes the pressure. The tube is placed in the anterior-inferior quadrant of the eardrum by ENT during an office visit. The tube falls out on its own in 6 months or so.

In this case, the tube is performing as expected. There is no bulging of the ear drum and no evidence of fluid in the middle ear space. The malleus is clearly visible. Notably, the tube appears to be on its way out of the ear drum, as expected. The annulus of the tube is no longer flush with the ear drum suggesting the process of extrusion. Here is an example of a completely extruded tube.
Here is the complete video exam:
Complete exam video
.

Acute Otitis Media (AOM)
A four-year-old female child is brought into the pediatric clinic by her father. She has had 3 days of a viral syndrome including cough, runny nose, and mild fever. Yesterday, she began to complain of right ear pain that seems to have been getting worse. The father has been treating the child with acetaminophen. The child has generally been in good health although the father reports occasional “ear problems.” On exam, the child looks uncomfortable but is alert and cooperative. This image of her right ear is obtained. What is your diagnosis and treatment?
The child has acute otitis media (AOM). Antibiotics should be considered.
Acute otitis media (AOM) is one of the top 3 reasons that children seek medical attention and the most common reason for antibiotic administration. This case describes a common situation, what appears to be a viral upper respiratory infection that develops into AOM. Although the child likely started with a viral infection, in a significant number of cases the ear infection also develops a bacterial component. For this reason, antibiotics are often considered for AOM.

Acute otitis media is diagnosed when bulging of the ear drum is present along with pain and potentially decreased hearing. In addition, there is often pronounced vasculature on the ear drum, as in this case. Compare this case of AOM to a normal eardrum below. Note that in the case of AOM, there is a loss of the bony landmarks due to the bulging of the ear drum. The bulging is caused by fluid in the middle ear space that can not drain because of Eustachian tube dysfunction.
Here is an article showing the natural history of AOM in images after the initiation of antibiotics.
Here is the complete video exam:
Complete exam video

Retained Hearing Aid Tip
A 57-year-old male presents to urgent care with an ear complaint. This image is obtained.
What is your diagnosis?
The patient has a hearing aid tip in his external ear canal.
Foreign bodies in the ear canal are a common presentation to the clinic. Besides hearing aid tips, it is common to see insects (ants, flies, ticks), beads, earrings, and popcorn kernels. The Wispr digital otoscope is very helpful in identifying the object and planning for its removal. In this case, the hearing aid tip was uneventfully removed with forceps.
WiscMed thanks Dr. Brittany Glenn of Cali Quick Urgent Care for this interesting case.

Bullous Myringitis vs Cholesteatoma Pearls
A 12-year-old male presents to the pediatric clinic for a well-child exam. The child and his parents have no concerns. He has no history of ear infections. The following image of his left ear is obtained. What is the diagnosis and treatment?
It appears to be asymptomatic bullous myringitis. It could also represent cholesteatoma pearls. Close follow-up is recommended.
This is an interesting case. An asymptomatic pediatric patient is here for a well-child visit with incidental discovery of apparent bullous myringitis (BM). BM may be considered to be on the “severe end” of acute otitis media (AOM). That is, AOM with additional features of infection. AOM generally presents with ear pain, decreased hearing, and signs of infection as seen in this image, that is; loss of bony landmarks, erythema (redness) along with bulging of the tympanic membrane (ear drum). The feature that separates BM from AOM is blistering. The diagnosis of BM is not definitive given the lack of symptoms experienced by the patient.

The other possibility is that the blisters actually represent cholesteatoma pearls. A cholesteatoma is an overgrowth of the epithelium of the tympanic membrane. The overgrowth can become a problem if it interferes with the proper functioning of the tympanic membrane or the middle-ear ossicles (bones).
It would a coincidence to have clear evidence of asymptomatic AOM (bulging of the ear drum) with incidental discovery of cholesteatoma pearls. For this reason, asymptomatic BM is the likely diagnosis. The child should return for re-evaluation in 1-2 weeks and if unchanged, be referred to ENT for evaluation of cholesteatoma. Given the lack of symptoms (pain, fever, decreased hearing), antibiotics are not indicated at this time.
WiscMed thanks Dr. Daniel Lapidius of Pediatric Affiliates for this interesting case. WiscMed also thanks Dr. Michael Poole of Georgia Ear, Nose, and Throat for his consult on this case. WiscMed highly recommends Dr. Poole’s book “Otitis: The Expert’s Diagnostic Guide.” Currently available at no cost on Apple Books.
Here is the complete video exam:
Complete exam video

Normal Ear Drum Anatomy
A medical student obtained this image using the Wispr digital otoscope. She would like your help in identifying the primary ear anatomy.

This is a healthy and normal ear. The eardrum (tympanic membrane) is the circular surface that dominates the image. The eardrum vibrates from sound waves. The vibration of the ear drum has to be transferred to the inner ear to produce electrical signals that we interpret as sound. The transfer of the vibrating eardrum to the inner ear is accomplished by three bones in the middle ear, these bones are “behind” the eardrum. Two of these bones can be seen in this image, the malleus, and the incus. The third bone, the stapes is not clearly visible in this image. The umbo is the distal end of the malleus that is generally centered in the ear drum. Finally, the chorda tympani nerve is also visible. This nerve provides taste sensation and secretory messages. It provides no innervation to the ear, it just happens to traverse the middle ear space.
Here is the complete video exam:
Complete exam video

Bulging Pars Flaccida
A two-and-a-half-year-old female is brought into the pediatric clinic by her mother. The child has had two days of viral symptoms including cough and congestion and now has a fever of 39 C. The child has been generally healthy with no history of ear infections. Multiple children at daycare have had similar symptoms. On exam, the child looks ill without being toxic. She is alert to activities in the room. Her lungs are clear. She has a cough and rhinorrhea. The following image of her right ear is obtained. What is your diagnosis?
The child has bulging of the pars flaccida portion of her tympanic membrane (ear drum) without evidence of acute otitis media.
This is a common clinical pediatric presentation. A collection of symptoms that most likely represent a viral infection of the upper respiratory system, but that could also lead to acute otitis media (AOM, middle ear infection). This case is particularly interesting because there is a clear bulging of the pars flaccida portion of the tympanic membrane (ear drum).
Recall that the pars flaccida is the “loose part” of the ear drum, and therefore the first to react to increased pressure in the middle ear. This can be caused by a crying, upset, breath-holding child. The Eustachian tube ventilates the middle ear space to the posterior nasal pharynx. You have observed this yourself when your ears pop in an airplane during descent. At the same time, the Eustachian tube can also pressurize the middle ear space if lung pressure is applied against a closed mouth and nose, known as the Valsalva maneuver. Children are good at performing the Valsalva maneuver when upset. The maneuver communicates the increased pressure in the mouth to the middle ear where it is externally observed as bulging of the pars flaccida.
The diagnosis of AOM relies on bulging of the complete tympanic membrane, the “angry donut.” Compare the image from this weeks case to an image of acute otitis media. Note that in the AOM case, the complete tympanic membrane is bulging and it is not possible to identify the malleus bone.
It is unlikely that this case represents developing acute otitis media. Developing AOM would generally include other signs of middle ear infection in addition to pars flaccida bulging such as air-fluid levels and purulence in the middle ear space. It’s possible, but unlikely, that this could be residual bulging from resolving AOM. See this Wispr University article for images of developing and resolving AOM. Most likely the observed bulging of the pars flaccida is due to a breath-holding child.
The child was diagnosed with a viral syndrome and the mother was given careful return instructions. Antibiotics were not indicated.
WiscMed thanks Dr. Daniel Lapidius of Pediatric Affiliates for this interesting case. WiscMed also thanks Dr. Michael Poole of Georgia Ear, Nose, and Throat for his consult on this case. WiscMed highly recommends Dr. Poole’s book “Otitis: The Expert’s Diagnostic Guide.” Currently available at no cost on Apple Books.
Here is the complete video exam:
Complete exam video

Acute Otitis Media (AOM)
A 6-year-old child presents to the pediatric clinic with several days of cough, throat pain, and now 12 hours of right ear pain. On exam, the child appears ill without being toxic, has rhinorrhea, a fever of 101.5F, and clear lungs. This image of the right ear is obtained.
The child has acute otitis media (AOM).
The hallmark of AOM is a bulging eardrum that often appears as an “angry donut.” The reason for the bulging is an infection that increases the pressure in the middle ear space which is behind the eardrum. It looks uncomfortable, and it is. Compare the annotated images of acute otitis media with a normal ear. In the case of the normal ear, you can clearly identify the malleus bone, the incus bone, and the chordi tympani nerve.
Treatment includes pain control with over-the-counter analgesics. Generally, antibiotics would also be prescribed. Children are more susceptible than adults to otitis media because their eustachian tubes are more horizontal. If the child has recurrent otitis media, ventilation tubes will often be placed.
Understanding normal ear anatomy is helpful to appreciate when something is abnormal. WiscMed has created a short video that explains normal ear anatomy and function.
Normal Ear Anatomy As Seen by an Otoscope

Eardrum Retraction
A 56-year-old employee of WiscMed was performing an examination on himself using the Wispr Digital Otoscope. An apparent “hole” in his eardrum caught his attention. He has no ear pain and no loss of hearing. He has never had ear trauma or a history of ear infections.
The WiscMed employee has retraction of the pars flaccida.
In this case, it presents as what appears to be a “hole” in the tympanic membrane. The hole is actually a retracted portion of the tympanic membrane that has a localized area of vasculature. The pars flaccida, as the name suggests, is the “looser” portion of the tympanic membrane that drapes across the superior portion of the malleus.
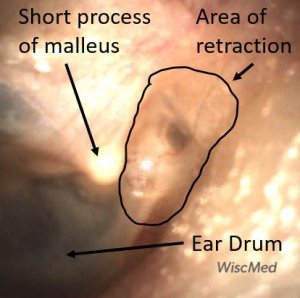
The tympanic membrane divides the external ear from the middle ear. The portion of the membrane that drapes across the malleus bone can become retracted for a number of reasons. One reason is a prior history of trauma or infections, the other is compressed geometry of the ear canal. In this case, the compressed geometry of the ear canal is causing a fold of the tympanic membrane that appears as a “hole.” This might be considered a pseudo retraction. Compare this case with another example of pars flaccida retraction and normal:
WiscMed thanks Dr. Michael Poole of Georgia Ear, Nose and Throat for his consult on this case and we highly recommend his book “Otitis Media” available currently at no charge on Apple Books.
Here is the complete video exam:
Complete exam video

Localized Thickening Of The Tympanic Membrane (Eardrum)
A healthy 24-year-old female presents for a routine clinic appointment. She has no complaints. She has no history of ear infections or trauma. She has normal hearing. Examination of her right ear with the Wispr Digital Otoscope reveals this image.
What abnormality do you note with the eardrum?
The patient has a localized thickening of her tympanic membrane (eardrum).
This appears as a “bubble” in the middle of the eardrum. You will also note that the cone of light from the otoscope is distorted by the thickening. Dr. Michael Poole has described this as a “fibrous disk” in chapter 5 of his excellent book, “Otitis: The Expert’s Diagnostic Guide.”

The tympanic membrane (eardrum) is comprised of three layers of tissue. The (1) outer cutaneous layer, the (2) middle fibrous layer, and the (3) inner mucosal layer. In the case of this patient, it appears that there is a localized thickening of either the outer cutaneous or middle fibrous layers. The cause of this is not known, but it does not seem to involve either infection or trauma. It is likely of embryologic origin. Multiple exams of this same ear have occurred over several years and the presentation has been stable.
In some cases, the thickening can be quite dramatic, and appearance may be confused with bullous myringitis. The distinction between the two is the complete lack of any symptoms with the layer thickness as opposed to significant distress (pain) and erythema (redness) associated with bullous myringitis. There is no apparent clinical significance associated with this finding. Here is another case featuring a fibrous disk.
The image also nicely illustrates both the malleus and the incus bones.
Here is the complete video exam:
Complete exam video

Bones Of The Middle Ear
A healthy 30-year-old male presents to the internal medicine clinic for a routine physical exam. The patient has no specific concerns during this visit. Examination of the left ear with the Wispr Digital Otoscope reveals this image.
Can you identify the three bones of the middle ear, the hammer (malleus), anvil (incus), and stirrup (stapes)?
In this beautiful image of a healthy and normal ear, it is easy to identify all three bones, technically ossicles, of the middle ear. The middle ear is the space behind the transparent eardrum. The bones of the middle ear are the malleus, incus, and stapes. Commonly referred to as the hammer, anvil, and stirrup. These bones are on “the other side” of the eardrum; they are in the middle ear. The eardrum separates the outer ear (the ear canal, open to air) from the middle ear. The eardrum is much like a common musical drum. Most of the surface, the pars tensa, is taught and responds to sound waves with movement.


The malleus (hammer) is attached to the eardrum and communicates the movement of the eardrum to the inner ear via the chain of bones; malleus, incus, and stapes. In many cases, the tympanic membrane (eardrum) is translucent enough that it is possible to identify both the malleus and the incus. Occasionally, you can also identify the stapes as in this example. The stapes is the bone farthest away from the ear drum which is why it is often not possible to see with otoscopy. You can see how the relatively long malleus acts as a lever to amplify small movements of the eardrum to the incus. The structure of the middle ear is an example of nature’s elegant biomechanical engineering.
At Wispr University we have an article on normal ear anatomy that can be helpful in understanding what you see during normal otoscopy.
Here is the complete video of the exam:
Complete exam video

Significant Exostosis
A 60-year-old male with a long history of windsurfing and other ocean sports undergoes an ear exam with the Wispr digital otoscope. Why is the patient’s tympanic membrane (eardrum) so difficult to see?
The patient has significant exostosis. This distorts the external ear canal and makes it difficult to visualize the eardrum.
Exostosis is an abnormal bony growth. The ear canal is a common location for this. Exostosis is caused by frequent exposure to cold water and is commonly seen in active water enthusiasts. Exostosis is not cancer, and generally, no action needs to be taken unless it is so severe that it leads to infection or hearing loss. It is a striking finding when first observed.

The patient reported otitis externa in the left ear about a week before the exam. Symptoms were reported as decreased hearing and a sense of fullness. It was treated with an antibiotic drop. If frequent infections occur, consultation with an ENT specialist would be appropriate.
The patient has bilateral exostosis, perhaps worse on the left side than the right side.
Here are examples of mild, moderate, and significant exostosis. Exostosis generally increases as the exposure to cold water continues.
Here are the complete video exams of the left and right ears:
|
Left Ear |
Right Ear |

Exostosis
A healthy 26-year-old pediatric resident physician stopped by the WiscMed booth at the Pediatric Academic Society (PAS) conference in Denver in April 2022. A demonstration of the Wispr digital otoscope was performed on her right ear. After seeing the image, the examiner concluded that the resident was a surfer. This was confirmed by the resident. What unique feature does this image have that supports that conclusion? Bonus question – what else can you infer about her life from this image?
The image shows mild exostosis (surfer’s ear).

Exostosis is an abnormal bony growth, in this case in the ear canal. At the tympanic membrane (TM, eardrum) the ear canal is generally “circle-like,” matching the geometry of the TM. You can see that in this photo the bony growth distorts that geometry. Here is an example of a normal ear canal and TM.
Exposure to cold water in the ear canal causes this overgrowth. It’s very common to see in surfers, open water swimmers, and kite surfers. The condition is ongoing, meaning that the more exposure to cold water, the more exostosis increases. In severe cases, bony growth can block the ear canal. This can lead to hearing loss and infection. The condition is benign. As long as there is no hearing loss, pain, or infections, the condition does not need to be addressed. If needed, definitive treatment is via surgery to remove the bony growth. Here is another example of exostosis.
What else can you infer from this image? The resident likely has a dog because of the “black hair” sign. It is unknown if the dog is also a surfer.

Here is the complete video of the exam:
Complete exam video

Middle Ear Effusion
A 4-year-old girl is transferred to the Emergency Department (ED) from Urgent Care (UC) due to concern for hemotympanum (blood behind eardrum) after a fall. Shortly before arrival, the child was climbing on playground equipment when she fell from approximately five feet and struck her face on the ground. There was no loss of consciousness and she cried immediately. The parents noted swelling and bruising around her nose.
She was taken to an UC where the medical provider noted that the left TM appeared very dark, raising his concern for a hemotympanum and basilar skull fracture. Since the child appeared otherwise well to the parents, they declined EMS transport and brought her to the ED via private vehicle. Upon arrival, the child was well-appearing with an exam notable for mild swelling and bruising to the upper nose. There was no nasal septal hematoma, but a moderate amount of blood was noted in the left nare. She had no scalp hematoma nor any midface, orbital, or dental injury. The following image of her left ear was obtained with a Wispr digital otoscope.
Which of the following is the most appropriate course of action based on physical exam and Wispr findings?
- Emergent head CT
- Emergent Neurosurgical consultation
- Emergent Maxillofacial CT
- Observation, reassurance, and outpatient follow-up as needed
The correct answer is “4” – Observation, reassurance, and outpatient follow-up as required.
Based on the Wispr exam, the initial concern for the hemotympanum is equivocal. The left ear has a middle ear effusion (MEE) and the fluid appears slightly darker than expected for MEE. It is unclear if this was the finding noted at the UC since it is pretty subtle and the “very dark TM” report is not supported by the Wispr images. Based on the child’s overall appearance and reassuring physical exam, it’s most likely the child has a middle ear effusion from a prior undocumented infection. A diagnosis of hemotympanum is less certain. As observed in a more severe case of epistaxis, blood from the nasopharynx may enter the middle ear via retrograde flow down the Eustachian tube. It is also notable that the TM of this patient is not bulging, unlike the previous WiscMed cases of hemotympanum associated with basilar skull fractures. Thus, the best answer based on physical exam and Wispr findings is observation, reassurance, and outpatient follow-up as needed with ENT after nasal swelling subsides.
The child was observed in the ED for an additional two hours, did not develop any worrisome symptoms, and was discharged home with relieved parents.
Here are the left ear and right ear video exams:
|
Left Ear |
Right Ear |

Acute Otitis Media
A 5-year-old male is brought into the pediatric clinic by his mother for evaluation of ear pain. The mother reports that three days ago the child developed a cough, runny nose, and congestion with a mild fever. She had been treating the symptoms with over-the-counter medicines. One day ago, the child began to complain about left ear pain. The child has a history of ear infections but has never needed ventilation tubes. The following image of the child’s ear is obtained with a Wispr digital otoscope.
What treatment is indicated?
The child has acute otitis media (AOM). Antibiotics should be considered
The child clearly has acute otitis media. The key diagnostic features of AOM include bulging of the tympanic membrane (TM), erythema (redness), and loss of all bony landmarks except the short process of the malleus. What’s interesting in this case is the presence of an air-fluid level. This suggests that as the inflammation in the middle ear space (behind the eardrum) developed, the air was trapped as the Eustachian tube prevented proper venting to the posterior nasopharynx. An air-fluid level can also be associated with a middle ear effusion (MEE). The difference between AOM and MEE is the presence of bulging. The bulging indicates increased pressure in the middle ear and therefore a non-functioning Eustachian tube.

Compare the images of AOM and MEE below. Both have air-fluid levels, but the MEE does not have bulging and the entire malleus is discernable.
Here is the complete video exam of the acute otitis media:
Complete exam video

Extruded Ventilation Tube
A five-year-old female is brought to the pediatric clinic by her mother with concern for ear pain. The child has a history of acute otitis media and had tympanostomy tubes placed about 6 months ago. For the past five days, the child has been complaining about right ear pain that seems to be getting worse. The mother has been using over-the-counter analgesics, but they have not been effective in the past day. This image of the right ear is obtained.
What is your diagnosis and what action should be taken?
The child has an extruded tympanostomy tube and acute otitis media. Antibiotics should be considered along with a referral to an ENT specialist.

The previously placed tympanostomy tube (ear tube, ventilation tube) has become extruded (fell out). This is an expected outcome of tube placement and generally occurs between 6 months and 1 year after placement. The eardrum generally heals quickly after the tube falls out although sclerosis may develop. The presence of bulging of the tympanic membrane (eardrum) indicates increased pressure in the middle ear space that is not being properly ventilated by the Eustachian tube. The bulging and pain likely represent acute otitis media (AOM). Considerations would include placing the child on antibiotics and referring to ENT for possible replacement of the tympanostomy tube.
Here is an example of a tympanostomy tube that is patent and still located appropriately in the eardrum.
Here is another example of an extruded tympanostomy tube.

Hemotympanum
A 3-year-old child is brought to a rural emergency department for evaluation of injury after being dropped by a “tall” family member, landing on his face. He cried immediately and seemed to be acting normally, however his parents became worried when he developed swelling and bruising over his right eye. He reportedly had no other findings to suggest additional injury. Given the eye bruising and mechanism, a CT of his head was performed that demonstrated a fracture through the superior orbital roof. The child was transferred to a pediatric trauma center for further evaluation where his Wispr examination revealed this image.
What is your diagnosis?
The child has hemotympanum (blood in the middle ear space).

The child in this case has a right-sided hemotympanum as demonstrated by the dark-colored effusion and tympanic membrane hemorrhages noted in the anterior superior and inferior quadrants. With traditional otoscopy, this finding is easily missed since it requires a well-directed light onto the TM. Without this proper lighting, not to mention the cooperation from an injured child, a clinician is unlikely to confidently identify the hemotympanum. However, with the images captured via Wispr, it is quite easy to distinguish “a dark TM” from the normal uninjured side. Due to this previously missed finding of hemotympanum, a temporal bone CT was ordered that demonstrated a subtle fracture and effusion (blood) within the mastoid air cells. Fortunately, all of the child’s injuries were felt to be non-operative and he was able to be discharged with otolaryngology follow-up to ensure that the hemotympanum resolved without affecting his hearing.
Here is another example of hemotympanum.

Acute Otitis Media (AOM) with Shangrination
A 6-year-old female presents to the pediatric clinic with ear pain. She has a history of acute otitis media (AOM), but no history of ventilation tubes. She has had the pain for about 6 days. The ear pain was preceded by viral symptoms including cough, congestion, and a sore throat. The parents have been treating the child with over-the-counter analgesics. They brought the child in because the ear pain does not seem to be getting better. On exam, the child appears well, although uncomfortable from the ear pain. Vital signs are normal and she is afebrile. The ear exam is shown. What action should be taken?
The child has acute otitis media with evidence of shagrination (cobble stoning). Antibiotics should be considered in consultation with the parents.
Acute otitis media (AOM) is diagnosed by the bulging tympanic membrane (TM, eardrum). The bulging represents pressure in the middle ear space due to fluid from inflammation. The presence of the fluid indicates that the Eustachian tube is not properly draining the middle ear space to the posterior nasopharynx. The bulging looks painful, and it is. The appearance is often described as an “angry donut” or “angry bagel.” This appearance is because the most distal part of the malleus, the umbo, creates the central dimple when the TM is under pressure. Compare this case to that of a normal eardrum.

In addition to features of AOM, the eardrum also appears to have shagrination1 (cobble stoning). Shagrination can be thought of as “stretch marks” on the eardrum and may be associated with improvement in the middle ear pressure. In other words, the stretch marks start to appear as the bulging subsides. This could indicate that the infection is resolving.
The choice of treatment, in this case, requires a discussion between the physician and the parents. Given the presence of shagrination, it would not be unreasonable to defer antibiotics and give careful return instructions. However, given the child has had symptoms for almost a week, it is most likely that the parents would prefer immediate treatment.
Here is another case on shagrination. And, here is a Wispr University article on the resolution of acute otitis media with the development of shagrination.
Here is the complete video exam:
Complete exam video
- Armengol, CE, and Hendley, JO, “Shagrination during Acute Otitis Media,” The Journal of Pediatrics, 2014;165:870.

Retraction Pocket
A 5-year-old female presents with complaints of congestion and cough. Her mother reports “at least a month” of symptoms. The child has a history of frequent ear infections and completed a course of amoxicillin three weeks earlier. In the ED she is afebrile and well-appearing. She has no ear complaints. Her Wispr exam of the left ear is shown. Upon review of the images with mother, she asks “How did that hole get there?”
The best answer to provide the child’s mother is:
- The child likely perforated her tympanic membrane (TM)
- The “hole” is a result of TM tube placement
- The finding is associated with negative pressure in the middle ear space
- “I don’t know”
The correct answer is “3.” The “hole” is actually retraction pocket.
While it is easy to see how the mother (and clinician) could mistake the dark oval area in the posterior-superior quadrant of the TM for a hole (rupture), this finding is an example of a mild retraction pocket (RP).

A retraction pocket is a localized invagination of the TM most often forming in the pars flaccida region (but not in this case). While the exact etiology is under debate, it is likely brought on by a combination of factors including chronic negative pressure and inflammation within the middle ear space. Thus, Eustacian tube dysfunction and recurrent or chronic otitis media are felt to play a role in its formation which may explain why they are much more common in children than adults. Here is an example of an eardrum retraction in an adult.
The malleus ossicle (bone) is a prominent feature seen on otoscopy. It is the first bone in the chain-of-three that translates sound waves to the middle ear.
While small RPs often resolve spontaneously and remain asymptomatic, there is the possibility of progression. In these instances, otorrhea, otalgia, erosion of ossicles, cholesteatoma formation, and hearing loss may occur. Since optimal management (also under debate) may involve surgical excision and tympanoplasty, follow-up with ENT is warranted to ensure the resolution of deeper or symptomatic RPs.
Here is the complete video exam:
Complete exam video
Urik M.; tedla M.; Hurnik P. Pathogenesis of Retraction Pocket of the Tympanic Membrane—A Narrative Review Medicina 2021, 57(5), 425; https://doi.org/10.3390/medicina57050425
Bunne, M.; Falk, B.; Magnuson, B.; Hellstrom, M. Variability of Eustachian tube function: Comparison of ears with retraction dis-ease and normal ears. Laryngoscope 2000, 110, 1389–1395.

Mild Bulging of the Eardrum
A 6-year-old female presents to the pediatric clinic with her mother. The child has had 3 days of viral symptoms including cough, congestion, and fever. She does not have any ear complaints. As part of the physical exam, this image of her right ear was obtained.
What is your diagnosis, and what intervention is indicated?
The child has mild bulging of her eardrum. Treatment with antibiotics might or might not be indicated. She likely has a viral infection causing her primary symptoms.
This is a common clinical situation. A child with viral symptoms and an ear exam that is equivocal for acute otitis media (AOM). There is clearly mild bulging of the eardrum, particularly the pars flaccida portion. However, the pars tensa portion is only mildly bulging. There is a slight dimple present at the umbo of the malleus. The short process of the malleus is still discernable. Here are examples of mild, moderate, and severe bulging. As the severity of the bulging increases, it becomes more difficult to discern the malleus ossicle.
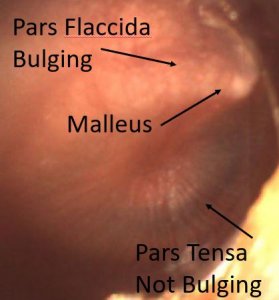
Mild bulging of the tympanic membrane
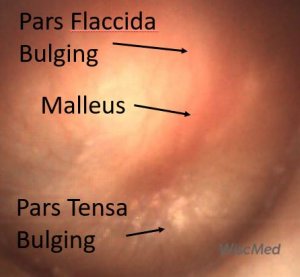
Moderate bulging of the tympanic membrane
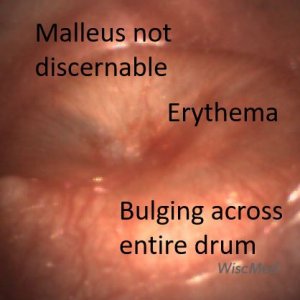
Severe bulging of the tympanic membrane
This article on Wispr University discusses the significance of bulging in the diagnosis of AOM. In the case of mild bulging, as seen in this case, secondary factors such as the presence of pain may help the practitioner to make the decision regarding treatment with antibiotics. Given that this patient had no pain, it would be reasonable to defer antibiotics while providing the family with careful return instructions.
Here is the complete video exam:
Complete exam video

Tympanic Perforation
A 6-year-old boy with a history of recurrent acute otitis media (AOM) presents with drainage from his left ear for one day. His father reports the child used to have frequent ear infections and had tubes placed a couple of years ago. Since that time, he has not had any ear infections although his hearing is somewhat diminished in the left ear compared to the right ear. He is supposed to be following up with his ENT for “some procedure”. His Wispr exam reveals this image and the likely indication for this procedure.
This child has a persistent tympanic perforation following the removal of his tympanostomy tubes (TM).
Additionally, there is mild otorrhea consistent with AOM. Upon further questioning, the child’s dad recalls a minor procedure last year when the TM tubes were indeed removed from both ears.
Persistent perforation is a known complication following TM tube placement, although the reported rates vary widely from 2% (Grommet type) to 24% (T-tubes). If the tubes are not expelled naturally, removal may be indicated after 18 to 24 months. Since most perforations close spontaneously, they may be observed up to a year before intervention with tympanoplasty or a variety of patching techniques. However, if left untreated perforations may cause conductive hearing loss and place the child at risk for recurrent infection. At his most recent ENT appointment, it was felt that he may require a myringoplasty due to the persistent perforation and diminished hearing.
Incidentally, the astute clinician will note the presence of the “Black Lab Sign” on the child’s Wispr exam. Father notes the family did in fact have a very loving Labrador retriever that frequently slept with the patient.
Here is the video of the exam:
Complete exam video

Fibrous Disk
A 16-year-old female is at her pediatric clinic for a routine appointment. She has no complaints. She has normal hearing and has never had ventilation tubes. The following image of her right ear is obtained. What abnormality do you notice? What intervention is indicated?
The patient has a fibrous disk centered over the umbo of the malleus.
This is a benign condition, and no intervention is indicated.

The tympanic membrane (eardrum) is comprised of three layers of tissue. The (1) outer cutaneous layer, the (2) middle fibrous layer, and the (3) inner mucosal layer. In the case of this patient, it appears that there is a localized thickening of either the outer cutaneous or middle fibrous layers. The cause of this is not known, but it does not seem to involve either infection or trauma. It is likely of embryologic origin. Dr. Michael Poole has named this condition “fibrous disk” and is well-described in Chapter 5 of his book “Otitis: The Expert’s Diagnostic Guide.”
Here is another example of a fibrous disk:
Here is the video of the exam:
Complete exam video

Foreign Body – fly in ear
A 16-year-old female presents with concerns of fever and shortness of breath. During the exam, the following image of her right ear was obtained.
The patient has a fly in her ear canal.
After seeing the image, the physician inquired further. The patient explained that about a week ago she was lying in bed when she felt something in her ear. It was disturbing to her so she sought assistance from her Mom. Her Mom could not see anything in the ear. However, the mother did extensive manipulation of the outside ear which caused the movement sensation to stop. It’s likely that the manipulation crushed the fly. The physician removed the fly uneventfully with a curette. Her fever and respiratory symptoms were attributed to a viral illness.
View some other examples of insects in the ear; ant, tick, spider.
Here is the complete video exam:
Complete exam video
WiscMed thanks Dr. Joao Mauricio Scarpellini for this interesting case. Dr. Scarpellini is a pediatrician in private practice in Rio de Janeiro, Brazil.

Foreign Body – Pencil Tip
A previously healthy 7-year-old male is brought to the pediatric clinic with concern for a foreign body in his ear. He had been in class, playing around by inserting a red pencil in his ear. The teacher became alarmed and told him to stop. When the pencil was removed, the tip of the pencil was missing.
The child has the tip of a red pencil in his ear.
Kids will find endless foreign bodies to insert in their ears. Tic Tacs, plastic parts, beads, more beads, and of course everyone’s favorite, popcorn. Removal techniques include forceps, glue tips, Katz extractors, and irrigation. The correct technique depends on the object and the level of cooperation of the patient. In young children, you will often have one chance to remove the object in the clinic. After one attempt, the child is often no longer cooperative. When this happens, sedation in the operating room is required. The Wispr digital otoscope is helpful in determining the position of the foreign body to help guide a removal technique, increasing the chance of first-attempt success.
In this case, the pencil tip was removed uneventfully with a lighted curette.
Here’s a video of the exam:
Complete exam video
WiscMed thanks Dr. Joao Mauricio Scarpellini for this interesting case. Dr. Scarpellini is a pediatrician in private practice in Rio de Janeiro, Brazil.

Bullous Myringitis
A 5-year-old male presents to the pediatric clinic with ear pain. The child recently started attending school and his father reports that several classmates have been diagnosed with a respiratory syncytial virus (RSV). Three days ago the child developed a cough, fever, runny nose, and congestion. The parents treated the symptoms with over-the-counter medications. Yesterday, the child developed ear pain. He continues to eat and drink and be active, although with less enthusiasm than is normal for him. The following image was obtained. What is your diagnosis?
The child has bullous myringitis.
This is a common clinical scenario. A pediatric patient with viral symptoms and then developing ear pain. Bullous myringitis is an infection of the middle ear, like acute otitis media, but distinguished by blistering on the tympanic membrane (eardrum).

With acute otitis media, the pressure inside the middle ear space from infection/inflammation causes the entire tympanic membrane to be “evenly” bulging. With bullous myringitis, bulging from the middle ear space is also present, but in addition, there are discrete blisters as seen here.
Compare the three examples below of a normal ear, an ear with acute otitis media, and an ear with bullous myringitis.
Treatment is focused on providing pain relief along with treating the underlying infection. An anesthetic such as topical lidocaine can be introduced in the ear canal to provide timely pain relief. Treatment of the underlying infection is the same as for acute otitis media.
Historically, bullous meningitis was thought to be caused by Mycoplasma pneumoniae. However, as Mellick(1) documents in his letter, it is a component of severe AOM whose underlying cause may be a number of infectious agents.
(1) Mellick and Verma, Letter, Pediatric Emergency Care, Volume 26, Number 12, December 2010

Quadrants of the Tympanic Membrane
A medical student obtained this image of a tympanic membrane (eardrum) and has asked for your help in identifying the quadrants and understanding their significance.
The quadrants of the tympanic membrane and their significance.
The first step in identifying the quadrants of the tympanic membrane (TM) is locating the malleus bone. The malleus is the first ossicle (bone) in the three-bone chain that transfers the motion of the tympanic membrane to the inner ear. The malleus is also a prominent landmark associated with the TM that helps to distinguish left vs right ear. The malleus always “points” to the face. In this example, the malleus is pointing up and to the left, so this must be the left ear.

Identifying the quadrants proceeds by drawing a line through the malleus. Since we now know that this is the left ear, this line separates anterior (front) from posterior (back).
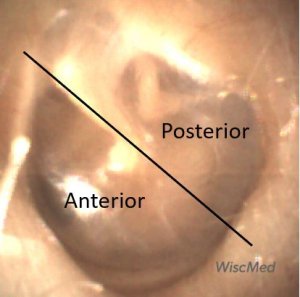
The next step in identifying the quadrants is to locate the umbo of the malleus. At the umbo a line is drawn perpendicular to the previous line separating anterior from posterior.
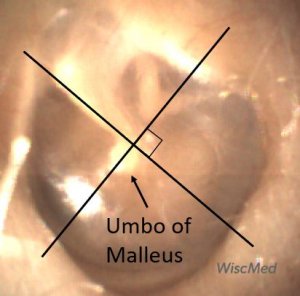
This new line separates superior from inferior. We now have all four quadrants of the TM identified.
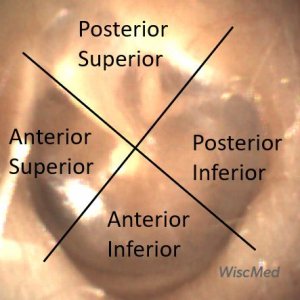
Now that the quadrants have been identified, the significance of each quadrant can be discussed.
Posterior Superior
This quadrant contains most of the pars flaccida portion of the tympanic membrane. This is the “looser” portion of the membrane that forms the “roof.” This is the area where middle ear pressure in the form of bulging is first evident, for example in acute otitis media. The posterior superior quadrant also contains the incus bone and the stapes bone. Sometimes the chordi tympani nerve can also be seen in this quadrant. This quadrant is where it is easiest to see TM movement when a patient performs a Valsalva maneuver. Ventilation tubes are not placed in this quadrant because of the risk of damage to the ossicles and chorda tympani nerve.
Anterior Superior
This quadrant is part of the pars tensa portion of the TM although a small portion of the pars flaccida is located in the most anterior superior portion of the quadrant. Behind this quadrant, in the middle ear space, is located the eustachian tube orifice. This tube provides pressure equalization across the TM by ventilating the middle ear space (the area behind the TM) to the posterior nasopharynx.
Anterior Inferior
This quadrant is entirely made up of the pars tensa. The promontory of the middle ear space is located approximately between this quadrant and the posterior inferior quadrant. The promontory is the outer rounded bulge from the cochlea.
Posterior Inferior
This quadrant is entirely made up of the pars tensa. The promontory of the middle ear spaces is located approximately between this quadrant and the anterior inferior quadrant. Part of the stapes ossicle terminates at the oval window behind this portion of the TM. This is also a quadrant to avoid when placing ventilation tubes.
Here is the complete video of the left ear exam:
Complete exam video

Ear Ventilation Tube
A 6-year-old male presents to the pediatric clinic for a well-child check. His mother does not have any concerns today. The child has a history of acute otitis media and had ventilation (ear) tubes placed about 3 months ago. The following image of the right ear was obtained.
What action needs to be taken today?
The patient has a patent, well-placed ventilation tube without evidence of infection. No action is necessary.
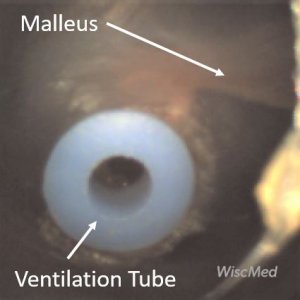
Ventilation tubes, also known as “ear tubes” and tympanostomy tubes, are commonly placed for cases of recurrent acute otitis media (AOM) and less commonly for chronic middle ear effusions (MEE). The tubes are placed in the anterior-inferior quadrant of the TM. This location is directly opposite the location of the Eustachian tube orifice in the middle ear. Tympanostomy tubes provide equalization of pressure across the TM. They essentially temporarily replace the job of a poorly functioning Eustachian tube. Small children are susceptible to Eustachian tube dysfunction because their anatomy causes the tube to be relatively horizontal, causing drainage challenges. As children grow, the Eustachian tube becomes more vertical, allowing proper drainage to the posterior nasopharynx. This partially explains why ear infections are so much more common in children than adults. In this case, the TM appears normal as does the malleus bone. The ventilation tube is well-placed and its annulus appears patent.
The ventilation tubes eventually fall out on their own, typically in 6 to 12 months. The tympanic membrane generally heals with no long-term hearing consequences. Occasionally, there is evidence of prior ear tub placement. Often, there is myringosclerosis of the TM which has no clinical significance.

Resolving Acute Otitis Media
A 3-year-old male presents for reevaluation 3 days after being diagnosed with acute otitis media (AOM). The mother reports that the child has had frequent ear infections in the past. 3 days ago, he presented to urgent care with fevers and left ear pain. Prior to the ear pain developing he had viral symptoms including congestion, cough and a sore throat. At the visit 3 days ago, he was placed on an antibiotic for AOM. The mother reports that today he is “back to normal,” with high energy and a good appetite. Examination of his left ear reveals this image. Is any further intervention necessary?
The child’s acute otitis media is resolving as expected. No further intervention is indicated. The complete course of prescribed antibiotics should be taken.
The child’s exam reveals evidence of resolving AOM. The short process of the malleus is partially discernable, although it’s definition is still not that of a normal ear. There is mild bulging of the pars tensa portion of the tympanic membrane (TM) (compare with significant bulging seen here) along with bulging of the pars flaccida portion of the TM. There is an air-fluid level present suggesting that the Eustachian tube has started to allow ventilation of the middle ear space. Overall, this image is consistent with the natural history of AOM resolution.
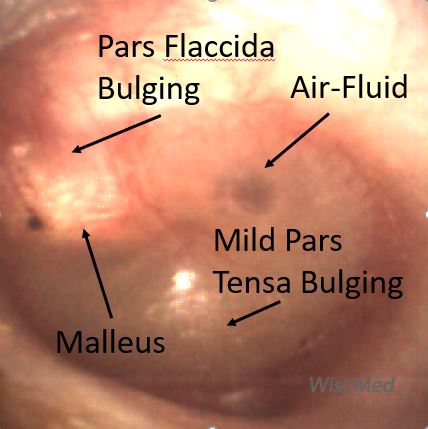
Here is a comparison of the patients left ear with resolving AOM and his normal right ear:
Here is the complete video of the left ear exam:
Complete exam video

Seborrheic Dermatitis
A 3-year-old male presents to the emergency department (ED) for evaluation of ear pain. Mom reports that he collided with an adult while on a trampoline two weeks ago when he was struck particularly hard by his “large” uncle’s knee in the temporal region. The child initially had a headache which has resolved. However, since the injury, he continues to complain intermittently of right ear pain that is worsened by lying down. He has not had fevers or other signs of illness. When mom spoke to his primary doctor’s office, they directed him to the ED for evaluation due to the concern for a head injury. In the ED, the child is very well-appearing without external signs of injury—no hematoma or ecchymosis. Wispr exam did not demonstrate hemotympanum but did reveal the likely cause of his ear complaint.
The child has seborrheic dermatitis of the external auditory canal.
While this child was sent to the ED given his reported head injury and ear pain, thankfully this was a historical red herring as the patient showed no signs or symptoms to suggest significant injury. On the contrary, Wispr exam shows that he has scaly, dry skin extending deep into the external auditory canals. In particular, his right external auditory canal (EAC) was filled with white-yellow exudative material. When commenting to the mom about the scaly findings, she noted that “he always has flaking in his scalp” as well. The last bit of additional information helped confirm the diagnosis of seborrheic dermatitis.
Seborrheic dermatitis is well-known by most clinicians to occur in the neonatal period, but this condition of inflamed, itchy skin can occur at any age. Commonly affected sites include the scalp, eyebrows, and posterior auricular areas but may include the ear canal as observed in our patient. While the differential diagnosis includes bacterial otitis externa (swimmer’s ear) or other forms of dermatitis (atopic or contact), the lack of pain with manipulation of the canal, no prior history of prolonged water immersion, and the presence of flaky scalp all support the diagnosis of seborrhea. It is interesting to note that the tympanic membrane (TM) of the right canal has patchy opacities but no bulging and normal malleus is visible. Presumably, the patchiness of the external surface of the TM is a consequence of having inflammation in the EAC and the lack of bulging or middle ear effusion (MEE) suggests there is no middle ear involvement. Treatment for this patient was steroid ear drops followed by clotrimazole ointment. This can be applied gently with a Q-tip and has the added benefit of a greasy barrier that will help calm the inflamed skin.
Here is the video exam of the right ear:
Complete exam video

Otitis Media with Effusion (OME)
An 18-month-old female is brought into the emergency department (ED) with concerns for vomiting, fever, and fussiness. The child had historically been well and is age-appropriate vaccinated. The symptoms began 2 days earlier. Symptoms initially included pulling at the ears, escalating to vomiting, poor feeding, and fever to 103 F. The parents treated the child with antipyretics but became concerned when the child seemed to be declining further. They brought her to the ED with a primary concern of dehydration. In the ED, she was found to have a brisk capillary refill, elevated heart rate and a fever of 102 F. Influenza and COVID tests were both negative. Urinalysis was also negative. This image of her right ear was obtained.
Would you start the child on antibiotics based on the history, exam, and imaging presented?
The child has Otitis Media with Effusion (OME)
Antibiotics are not indicated based on the imaging obtained from the right ear.
The right ear is not normal. The abnormality is the air-fluid levels in the middle ear space. However, there is no bulging of the tympanic membrane (eardrum), and the malleus ossicle is discernable. All of these features indicate a properly functioning Eustachian tube, which drains and ventilates the middle ear space to the posterior nasal pharynx. The air-fluid levels are from inflammation, likely from a viral syndrome based on the child’s history and exam.

Day 0 right ear exam with annotation showing middle ear effusion (MEE)
This is the same patient as presented in this case where the other ear, the left ear, did progress to acute otitis media (AOM). You can see on the annotated image below the striking difference.
Compare the annotated right ear (above) and left ear (below). There is an obvious difference between a MEE and AOM.

Day 1 left ear exam with annotation showing acute otitis media (AOM)
Here is the complete video exam.
Complete exam video

Progression to AOM
An 18-month-old female is brought into the emergency department (ED) with concerns for vomiting, fever, and fussiness. The child had historically been well and is age-appropriate vaccinated. The symptoms began 2 days earlier. Symptoms initially included pulling at the ears, escalating to vomiting, poor feeding, and fever to 103 F. The parents treated with antipyretics but became concerned when the child seemed to be declining further. They brought her to the ED with a primary concern of dehydration. In the ED, she was found to have a brisk capillary refill, elevated heart rate and a fever of 102 F. Influenza and COVID tests were both negative. Urinalysis was also negative. The following image of her left ear was obtained. Would you start the child on antibiotics based on the history, exam, and imaging presented?
This is a typical case seen in the pediatric emergency department. A previously well child with signs and symptoms often associated with a common and benign viral infection. The pressing issue is to rule out treatable conditions. In a female child this age, those conditions would commonly be a urinary tract infection (UTI) or acute otitis media (AOM). As noted, she did not have a UTI on urinalysis.
Given the image found on Wispr otoscopy, the question of treatment for AOM is not straightforward. The left ear is clearly not normal. There is evidence of purulence in the middle ear space and the pars flaccida portion of the tympanic membrane (TM) is bulging. However, the malleus ossicle is still discernable, and the bulging of the pars tensa portion of the TM is minimal. In addition, there is an air-fluid bubble present indicating that the Eustachian tube is still functioning and suggesting a middle ear effusion (MEE).

Day 0 left ear exam
In consultation with the mother, the decision was made not to start antibiotics for AOM at this time.
The patient re-presented to the pediatric clinic the next day as symptoms did not improve.
The following image was obtained:

Day 1 left ear exam
On this serial exam, the disease process in the ear has progressed. The bulging of the entire eardrum is significant indicating increased pressure in the middle ear space and a poorly functioning Eustachian tube. There is increased purulence behind the tympanic membrane. A small air-fluid bubble is still visible, likely air trapped previously and not an indication of a properly functioning Eustachian tube.
With these findings, the child was placed on an antibiotic. She had rapid improvement in her symptoms within a day.
This case shows the importance of careful consultation with family members about the natural history of disease and strong encouragement to return for evaluation if symptoms worsen.
Here are the day 0 and day 1 video exams:
|
Left Ear – Day 0 |
Left Ear – Day 1 |

Foreign Body – Tic-Tac
A 10-year-old boy with mild autism presented to the emergency department (ED) with concern for a foreign body in his ear. As he walked past the physician computer stations, he was heard saying “I don’t know how they are going to get it out. It’s really far in there.” Upon evaluation, the child reported that he placed a tic tac in his right ear approximately an hour prior to arrival. His mother attempted to flush the ear with water, but this was unsuccessful in removing the object. Wispr otoscopic exam demonstrated that the child was correct in his assessment that the tic tac was indeed very deep in the external auditory canal (EAC).
Whether placed intentionally by a young child or as a consequence of sharing the earth with insects or because we listen to music, ear foreign body (FB) is a common chief complaint. Fortunately, successful removal can be facilitated by an understanding of the EAC anatomy, attention to patient comfort, and a steady hand.
The EAC is much more than a simple conduit connecting the outer ear from deeper structures. As a highly innervated channel that funnels sound waves and protects delicate middle ear tissues, the EAC anatomy can make visualization and retrieval of FBs challenging. Two such considerations encountered in this patient include canal orientation and anatomic narrowing.
Initial examination revealed the FB to seem anterior with the curvature of the canal partially obscuring the tic-tac. This curvature was easily straightened with gentle upward and posterior traction on the external ear and greatly minimized (but did not eliminate) the obstructing view. The tic-tac was still not completely visualized due to another normal attribute of the EAC-narrowing of the canal near the cartilaginous-osseous junction that becomes the frequent site of FB entrapment. Occasionally unsuccessful attempts at removal (or small fingers) may push the object past this junction and deeper into the canal, making retrieval even more difficult. This is likely to have been the case with our patient as the oblong tic tac appears to have been pushed inward, allowing it to rotate nearly vertical once past the narrowing. This orientation foiled initial attempts using the cyanoacrylate (super glue) technique as the force required to remove past the narrowing was too great. Fortunately, the child was remarkably compliant and ultimately tolerated removal with a micro-forceps borrowed from the ED’s plastic surgery tray. Following removal, he happily requested a picture of the tic tac to show his friends.

Here is the complete Wispr otoscope video of the exam:
Complete exam video

Acute Otitis Media (AOM)
A 16 month-old child is brought into the emergency department (ED) for evaluation of congestion, cough, and fever. The parents report the child has had nasal congestion and cough for the past 4 weeks with an occasional “day or two” of improvement. They are concerned because he has seemed chronically congested ever since starting daycare a little over a month ago. He was seen in the urgent care (UC) earlier in the evening and diagnosed with sinusitis. The UC also noted, “fluid behind ears without bulging.” Covid, influenza, and RSV tests were all negative, so he was sent home with a prescription for an antibiotic to treat presumed sinusitis. The child seemed irritable after returning home, so his parents decided to have him evaluated again.
Physical exam was notable for a well-appearing child with copious nasal drainage and clear lungs without any increased work of breathing. Wispr otoscopic exam revealed the following from the right ear.
The child has acute otitis media (AOM).
The case of the Congested Daycare Attendee has become a common theme over the past few months as increasing numbers of children return to daycare after missing out on natural immunity exposures during the height of the Covid pandemic. Fortunately, most cases of “continuous congestion” are simply uncomplicated overlapping viral URIs requiring parental reassurance and supportive measures. However, most clinicians recognize that co-infections are common, particularly when signs or symptoms are prolonged or worsening beyond the usual URI time course of 5-7 days.
A PubMed search reveals multiple investigations demonstrating that acute otitis media (AOM) frequently accompanies URIs. The key features of AOM include loss of malleus definition, bulging, and to lesser extent erythema. While the primary pathogenesis is felt to be secondary to Eustachian Tube (ET) dysfunction which decreases the ability to clear nasopharyngeal bacteria from the middle ear space, anatomic characteristics of short, horizontally-oriented ETs as well as their multitude of viral exposures make young children particularly vulnerable. In fact, a 2007 study published in Pediatrics, found that AOM occurred in 30% of pre-school-aged children with URI symptoms1. Thus, in our patient with URI symptoms and bulging on Wispr exam (likelihood ratio of 51), there is a whopping 97% probability of AOM. While it is less certain that he has sinusitis as diagnosed earlier in the night, an antibiotic was clearly warranted to treat his AOM.
Here is the video of the complete exam. Note that only a brief “flash” of the bulging ear drum is seen. This shows the power of the Wispr otoscope. Using video mode of the Wispr otoscope, the provider can focus on the exam without having to “process” what is being seen. Reviewing and scrubbing the video afterwards isolates the image of interest, clearly showing AOM.
Complete exam video
1 Krystal Revai et al. Incidence of acute otitis media and sinusitis complicating upper respiratory tract infection: the effect of age Pediatrics. 2007 Jun;119(6)

Significant Cerumen
A 30-month-old female presented to her pediatrician with concern for fever. The mother reports several days of cold-like symptoms including cough and congestion. Earlier in the day, the child developed a temperature of 102.2 F. She is fussy but continues to eat and drink. The mother has been treating the symptoms with over-the-counter antipyretics. On exam, the child looks ill without being toxic. She is well-hydrated, alert, and easily comforted in her mother’s arms. The child had a significant amount of ear wax. The following image was obtained with the Wispr digital otoscope without having to remove any of the wax.
The child’s ear is normal.
This case demonstrates the power of the Wispr digital otoscope. Even the youngest patients can have a significant amount of cerumen (ear wax). This often causes almost complete obstruction of the ear canal and blocks visualization of the tympanic membrane (TM). To properly diagnose ear pathology, a full view of the TM must be obtained. Because of the unique geometry of the Wispr Speculum, it is often possible to navigate through a “window” in the ear wax to obtain a view of the TM. That was the situation in this interesting case. Although the image is slightly blurry, it is still easy to determine that this is a normal ear. The malleus is clearly visible and there is no erythema or bulging that would be associated with acute otitis media (AOM).
The complete video shows the pediatrician carefully advancing the Wispr otoscope through a small window in the cerumen and obtaining a diagnostic view of the TM. In this case, the TM is normal, and no treatment is required. It is likely the child has a benign viral infection and can be sent home with careful return instructions.
Complete exam video

Myringosclerosis
A healthy 42-year-old male presents for a routine physical examination. He has no concerns to report during this visit. During the exam, the following image was obtained with the Wispr digital otoscope.
The patient has myringosclerosis.

Myringosclerosis is commonly seen during routine ear examinations. It represents deposits of calcium in the layers that make up the tympanic membrane (TM, eardrum). It is commonly associated with the patient having a history of ventilation tubes. It can also be related to a history of pathology such as acute otitis media (AOM). Although sclerosis appears dramatic, it is of little clinical concern and generally does not affect hearing to any significant extent. No treatment is required. Compare the TM in this case with the pristine TM in this case.
Here is the video of the exam:
Complete exam video

Acute Otitis Media (AOM)
A 19-month-old male is brought into the emergency department by his mother with concern for fever and fussiness. The child’s daycare was recently reopened after COVID protocols were deemed sufficient for the children’s safety. The mother reports that 3 days ago the child began to develop a cough and runny nose. For the past day, the child has had a temperature as high as 102.5 F. The mother has been using antipyretics for the fever and pushing fluids. On exam, the child appears sick without being toxic. He appropriately resists the exam and is easily comforted in his mother’s arms. His lungs are clear and he is mildly tachycardic. Capillary refill is less than 1 second. This image of his right ear is obtained.
The child has acute otitis media (AOM) of the right ear.
For much of 2020 and 2021, very few cases of viral syndromes in children were seen in primary care. This is presumed to be because of the effect of social distancing in reducing respiratory infections. Starting in the late summer of 2021, this situation has changed markedly as social distancing and home isolation have ended. Many ill children are presenting to primary care for evaluations such as this one. Although this child was not tested for a specific infectious agent, it’s a good bet that he has respiratory syncytial virus (RSV). RSV, although a virus, often leads to bacterial co-infection in the middle ear. Because of this, AOM is often treated with antibiotics.
Often in the case of an infection, both ears will have evidence of AOM. In this case, the child’s left ear was normal.
This provides a good opportunity to compare a normal ear to AOM in the same patient at the same time.


Here are the complete videos obtained from the child’s left and right ear exams:
|
Left Ear Video |
Right Ear Video |

Stapes Bone
A healthy 30-year-old female had a demonstration of the Wispr digital otoscope at the 2021 American College of Emergency Physicians Scientific Assembly (ACEP). This image of her ear was obtained.
Can you identify all three bones of the middle ear?

Bones of the Middle Ear
This is a beautiful example of a normal and healthy ear. What’s particularly notable in this image is the ability to see all three bones of the middle ear through the transparent tympanic membrane, the malleus, incus, and stapes, commonly called the hammer, anvil, and stirrup. It’s usually not possible to see the stapes as it is the deepest bone in the middle ear space. The stapes connects the incus to the oval window of the inner ear, allowing the mechanical energy of the tympanic membrane to be communicated to the fluid in the inner ear. The malleus is almost always visible except in cases of distorted anatomy such as from acute otitis media. The incus is often visible, but normal differences in anatomy can hide this bone, too.
More information on the anatomy and bones of the middle ear is available at Wispr University.
Here is a video of this ear exam:
Complete exam video

Foreign Body – Ear Bud
An emergency physician visited the WiscMed booth at the 2021 American College of Emergency Physicians in Boston. A demonstration of the Wispr was performed on his ear. This image was obtained.
The emergency physician has a retained foreign body in his ear.
This was a surprising finding to both the emergency physician (EP) and to Alex Bach, the WiscMed staff member who discovered the foreign body during the routine demonstration of the Wispr digital otoscope. After seeing the foreign body, the emergency physician had this to say:
“I’m ashamed to say that has likely been in my ear since August 2018. I used to run with in-ear headphones and one day part of it broke off in my ear. I thought I got it out but started to develop ear pain a few days later. I had my girlfriend (who is an Internal Medicine resident!) look in my ear with a cheap otoscope I owned from medical school at one point and she said she didn’t see anything (I have confronted her about this and informed her I plan on suing). For a long time afterwards I would have intermittent ear pain made worse with manipulation or if I was exercising or sweating. For a while I could not sleep on my right ear. I thought I had ruled out foreign body based on my girlfriend’s exam and was attributing my symptoms to bruxism. Stereotypically I never sought medical care. My ear feels a lot better now. Really glad I came across your booth!”
WiscMed staff had a good laugh at his good-natured “history of present illness.”
Here are several other examples of foreign bodies from devices designed for use in the ear. It makes one question why a manufacturer would ever design something for the ear that has a removable tip at the end!
The foreign body was uneventfully removed with alligator forceps at the WiscMed booth. This was perhaps one of the few times a needed medical procedure was performed at a national trade show. After removal, there was mild irritation of the external auditory canal, but otherwise, the tympanic membrane was normal.

Foreign Body Removed
Here is a complete video of the exam. Interestingly, it is possible to see a normal malleus “thru” the annulus of the retained foreign body.
Complete exam video

Shagrination or “Cobble Stoning”
A 16-month-old toddler presented to the emergency department with three days of nasal congestion and low-grade fever. The child had been otherwise well with only a mild cough. Due to a respiratory syncytial virus (RSV) exposure at daycare, his mother brought him for evaluation. His respiratory exam was reassuring with only the occasional mild wheeze and no increased work of breathing. Examination of the left ear revealed this finding.
This patient has the classic appearance of shagrination or “cobble stoning” of the tympanic membrane (TM).
The roughened appearance, shagrination (cobble stoning) of the TM is thought to occur during the course of acute otitis media (AOM) as the bulging membrane begins to return to its normal position as fluid in the middle ear recedes. While the exact pathophysiology is not clear, this finding reminds us that the TM is not a single homogeneous band of tissue but rather a multi-layered complex composed of epithelial (continuous with the external canal), fibrous (middle radial layer), and mucosal (continuous with the lining of the middle ear) cells.
Armengol and Handley published images of 17 children with AOM who either developed or presented with shagrination1. Follow-up images indicated that resolution of bulging typically occurred within the 1-2 days, suggesting that shagrination indicates the decompression of the middle ear space (think of the wrinkles in a deflated balloon) with a resolution likely to occur soon thereafter. Here is another example of shagrination.

Shagrination – cobble stoning additional view
As can be attested by many of the Wispr cases, the use of digital otoscopy facilitates not only the diagnosis of AOM but also provides opportunities to evaluate the significance of physical findings. In the Armengol paper, digital otoscopy demonstrated resolution of AOM findings within 1 to 2 days following the appearance of cobblestoning, including in three patients who did not receive antibiotics. While further studies in a larger cohort will be helpful, this suggests that the appearance of shagrination may herald spontaneous resolution and allow antibiotics to be avoided or curtailed in these patients. For further information, here is a case study of resolving AOM. In this study, shagrination appears on day 8.
Here is the complete video exam from this patient.
Complete exam video
- Armengol, CE, and Hendley, JO, “Shagrination during Acute Otitis Media,” The Journal of Pediatrics, 2014;165:870.

Extruded and Encrusted Ventilation Tube
An otolaryngology (ENT) resident stopped by the WiscMed booth at the 2021 ENT OTO Experience conference in Los Angeles, CA to experience the Wispr Digital Otoscope. The Wispr Digital Otoscope was used to perform an exam on her right ear. This image was obtained. What is your diagnosis?
The resident has an extruded and encrusted ventilation tube.
After obtaining this image and further history, the ENT resident endorsed having a tympanostomy (ventilation) tube placed in her right ear about a year ago for what was described as an effusion. Generally, an effusion would not be an indication for ventilation tube placement, but further information regarding the diagnosis resulting in the tube placement was unavailable. Tympanostomy tubes are generally placed in cases of repeated otitis media with eustachian tube dysfunction. The tubes are placed in the anterior inferior quadrant of the pars tensa, which lines up nicely with the Eustachian tube in the middle ear. They generally “fall out” on their own in about a year. Here is another example of an extruded ventilation tube.
Take a look at the complete video of this exam which demonstrates the power of the Wispr Digital Otoscope to help with diagnosis. Note how the distal camera on the Wispr is able to obtain a clear view of the annulus of the ventilation tube, confirming the object. The ventilation tube is most likely encrusted with keratin and cerumen (ear wax) which is why the nature of the object was initially unclear.
Complete exam video

Perforation of the Tympanic Membrane
A 27-year-old otolaryngology (ENT) resident stopped by the WiscMed booth at the 2021 ENT OTO Experience conference in Los Angeles. He knew that he had an “interesting finding” in his right ear and invited WiscMed staff to examine him. This image was obtained. What is your diagnosis?
The ENT resident has a perforation of his tympanic membrane.
The resident obtained the perforation to his tympanic membrane from a wipe-out during wakeboarding. The perforation never healed. Interestingly, he indicated that he had no decrease in hearing from the right ear. The defect to the tympanic membrane is located roughly in the same location where a ventilation tube would be placed in the case of chronic middle ear infections (acute otitis media), the anterior-inferior quadrant of the eardrum. A concern regarding a persistent perforation to the TM would be an infection from swimming. The resident did not indicate any problem with infections. In some scenarios, myrinogplasty may be recommended to repair the perforation.

This is an example of a larger perforation to the tympanic membrane.
Here is a video of the complete exam:
Complete exam video

Middle Ear Effusion
A college student has had congestion, runny nose, and a cough for several days. She then developed ear pain. She was tested for COVID and found to be negative. This image was obtained. Would you initiate antibiotics? Which ear is this?
The student has a middle ear effusion, antibiotics are not indicated. It is the left ear.
This is a common clinical scenario. Ear pain following several days of viral symptoms. The key to diagnosing a middle ear effusion is the presence of fluid and air-fluid levels behind the tympanic membrane. In addition, in an MEE the eardrum is not bulging as in acute otitis media (AOM). The presence of air-fluid levels indicates the Eustachian tube is functioning correctly, ventilating the “other side” of the tympanic membrane, or the middle ear space.

You can tell this is the left ear as the malleus bone always points towards the face.
Here is another example of a middle ear effusion.
See the video of the complete exam of the left ear:
Complete exam video
WiscMed thanks Anna Grasee of the University of Minnesota for this interesting case.

Foreign Body – Earring
A 19-year-old woman presents to the emergency department with concern for a foreign body in her left ear. She reports that she was lying in bed while touching her earring when a piece of the earring fell into her ear. She does not have any change in hearing, and she does not report any pain. She did not try to remove the earring herself other than tilting her head to the left side “abruptly.” This image is obtained.
The patient has a decorative piece from an earring in her left ear canal.
Foreign objects in the ear are commonly seen in the emergency department and the pediatric clinic. The WisprDigital Otoscope makes visualization and confirmation of the foreign body straightforward. The tricky part is removal of the foreign body. This case illustrates the challenge. The earring piece is deep in the canal, and awkwardly shaped. Possible removal strategies include irrigation, suction, forceps, or a curette. In this case, a stainless steel speculum was used to straighten the ear canal and allow for the removal of the earring piece with a curette.
Here is a photo of the removed object.

Earring Piece Removed
Here is the complete video of the exam:
Complete exam video

Otitis Externa and Mild Acute Otitis Media
A 26-year-old male presents to the emergency department at 1 am complaining of right ear pain. He reports the pain started about three days ago and has gradually gotten worse. He’s used ibuprofen and acetaminophen for the discomfort which has been partially helpful. He has not had any other symptoms – no fevers, cough, congestion nor rhinorrhea. He indicates he swam in the local lake about a week ago. He does not have any history of ear infections. This image of his right ear was obtained.
The patient has both otitis externa and mild acute otitis media.
This is a common clinical case. Ear pain with features on exam consistent with both otitis externa and acute otitis media (AOM). Regarding the otitis externa, there is clear inflammation of the external ear canal. This appears as the “rough” and red ear canal. Often, otitis externa will also have significant purulent discharge, as in this case. Regarding AOM, there is mild bulging of the tympanic membrane. In this case, the bulging is limited to the pars flaccida portion of the eardrum. AOM can have various levels of bulging and can be marked, as in this case.

In this case, treatment consisted of a systemic antibiotic for AOM along with antibiotic ear drops for the otitis externa. When using the ear drops, it’s important to use ear wicks so that the drops are introduced deep into the external canal.
Here is the recorded video exam of this patient:
Complete exam video

Acute Otitis Media
A 13-month-old male is brought in by his parents with concern for fever and fussiness. They report that the symptoms began about 3 days ago with a cough and runny nose. The infant’s temperature has been as high as 39 C at home and he has responded well to antipyretics. The child continues to drink, but with less enthusiasm. He continues to have wet diapers. He is up-to-date on immunizations. The mother works in the hospital and is concerned about the possible transmission of COVID to her son although no one else in the family is symptomatic. On exam, the child is well-appearing. He drools, has brisk capillary refill, and appropriately resists the exam with surprising ingenuity and strength. He is easily comforted in his mother’s arms. Examination of his right ear reveals this image.
The child has acute otitis media.
The Wispr Digital Otoscope image clearly reveals acute otitis media. The key characteristics are bulging (angry doughnut), erythema (redness), and loss of bony landmarks. Laboratory testing included Respiratory Syncytial Virus (RSV) and COVID swabs. COVID came back negative, but the RSV was positive. This is a common scenario in the late summer and early fall of 2021. For much of the COVID pandemic, RSV was rarely seen. It is now prevalent and the frequent cause of presentation to primary care. A reasonable question would be given that RSV (a virus) is positive, should antibiotics be initiated? Often with RSV, there is bacterial co-infection in the middle ear space. For this reason, even with a positive RSV diagnosis, consideration of antibiotics with acute otitis media is appropriate.
Notable with this child, and any grumpy child is the challenge of obtaining a good ear exam. The power of the Wispr digital otoscope is its ability to not only access the smallest ear canals but also its ability to record the exam. With the exam being recorded, the provider can focus on accessing the tympanic membrane without having to worry about mentally processing the view in real-time. After the exam, the video can be reviewed and frames of interest exported for discussion with the family or inclusion in the medical chart.
Here is the recorded video exam of this patient:
Complete exam video

Foreign Body – Hearing aid tip
A 72-year-old woman arrives in the emergency department concerned that a piece of her hearing aid is lodged in her ear canal. She explains that when taking the hearing aid out of her left ear, she noted that the rubber tip at the end was missing. She shows the right hearing aid with the rubber tip present and compares it to the left hearing aid with the left tip absent. This has not previously happened to her. She is accompanied by her daughter who enthusiastically explains that they tried to remove the rubber piece with pliers but were unable to do so. She offers to let the examining physician use the pliers which was politely declined. This image of the ear was obtained.
The patient has a retained portion of her hearing aid in the external ear canal.
This is a frequently encountered situation – a retained portion of the hearing aid in the ear. It makes one question the engineering expertise that placed a removable rubber tip at the end of a device that is placed deep in the ear canal! Using the Wispr digital otoscope, the foreign body was easily visualized. It was a simple matter to remove the rubber piece using alligator forceps. After removal, there was no evidence of trauma to either the external canal or the tympanic membrane. There is cerumen (ear wax) present at the 3 o’clock position.
This is the foreign body that was removed:
Here are the complete videos with the hearing aid piece in the canal, and after removal:
|
Foreign Body – hearing aid tip |
After removal of foreign body |

Bilateral Hemotympanum
A 15-year-old female presents to the ED (Emergency Department) with a chief complaint of epistaxis (nose bleed). She reports her nose began bleeding while at band practice, while playing the tuba, three hours earlier. The bleeding was quite profuse and did not stop despite several rounds of direct pressure. The teen became quite unsettled when she noticed her “eyes bleeding” so her parents brought her into the ED for evaluation. Aside from mild seasonal allergies and an occasional nose bleed associated with dry air, she has no other significant medical history.
In the ED, the patient was found to have active bilateral nose bleeding as well as a small amount of dried blood below her right eyelid. After placement of Afrin-soaked cotton balls into both nostrils and application of a nasal clamp for 30 minutes, the bleeding stopped. Following removal of the packing, prominent Kiesselbach’s plexuses were visible but her nasal passages were clear without clots or evidence of posterior bleeding. The patient expressed relief that the bleeding had stopped but noted that she was now experiencing slightly muffled hearing. Her Wispr exam revealed the cause for her new complaint. Here are images from both ears:
Wispr exam demonstrates bilateral hemotympanum without bulging or perforation.
While hemotympanum is well-known to occur in the setting of head trauma, a number of other scenarios may result in blood accumulating within the middle ear space. In our patient, the source of the hemotympanum is blood from the anterior nasal septum flowing posteriorly into the Eustachian Tube. As a conduit from the middle ear space to the nasopharynx, the Eustachian tube lacks a valve system to prevent such retrograde flow. While there are case reports of spontaneous epistaxis resulting in hemotympanum, it is much more likely to occur in the setting of nasal packing or prolonged bleeding. An interesting clue that our patient experienced such retrograde movement of blood was her additional report of bleeding from her eyes. This unusual complaint suggests there was enough pressure generated during her attempts to stop the epistaxis such that blood was forced up the nasolacrimal system and exited the tear ducts!
Here are the complete videos obtained of the left and right ear exam:
|
Left Ear Video |
Right Ear Video |

Acute Otitis Media
A previously healthy 6-year-old female presents to the pediatric clinic for ear pain. Her mother reports that three days ago she developed a sore throat followed by a cough, runny nose, and fatigue. She recorded a temperature of 101.5 F (38.6 C) at home that responded well to antipyretics. Yesterday the child began to develop left ear pain. She had a history of ear infections as a toddler, but none recently. No history of ventilation tubes. The mother reports that siblings at home had similar symptoms without the ear pain that have since resolved. This image of the left ear is obtained with the Wispr digital otoscope.
The child has acute otitis media (AOM).
This is a classic presentation of acute otitis media (AOM) – a prodrome of viral symptoms followed by ear pain. The image obtained is also a textbook characteristic of AOM. The notable features of this presentation include bulging of the eardrum, erythema (redness), and loss of the typical bony associated with the tympanic membrane (eardrum). The dimple seen in the bulging doughnut of AOM is due to the umbo of the malleus.
Compare a normal ear to this ear with AOM.
Treatment of AOM would typically be a course of oral antibiotics.
Here is the video exam of this case:
Complete video of exam

Mild Acute Otitis Media (AOM)
A 34-year-old female presents to the emergency department complaining of left ear pain. She reports that the discomfort began a day ago. She had previously had mild viral symptoms including congestion, headache, and malaise. She reports a sensation of fullness in her left ear along with decreased hearing. This image of her left tympanic membrane is obtained.
The patient has mild acute otitis media (AOM).
The AOM in this case is involving only the pars flaccida of the tympanic membrane. The pars tensa and the malleus are still discernable. This would generally be considered early and mild AOM. Given the clear presence of bulging of the tympanic membrane along with discomfort, a course of oral antibiotics would be reasonable.
Compare these three different cases of acute otitis media (AOM) ranging from mild to severe. With each increasing level of severity, more of the normal anatomy of the tympanic membrane is lost. For example, in the case of severe AOM, the malleus is no longer discernable due to the distension of the tympanic membrane.
Here is the video exam of the mild AOM:
Complete video of the exam

Hemorrhagic Bulla
A previously healthy 5-year-old male presents to the emergency department complaining of left ear pain. Four days ago, the child had a cough and sore throat. Yesterday, he began to develop a fever to 101.5 F and left ear pain. The mother has been treating with ibuprofen and acetaminophen. She is concerned that his symptoms are not getting better. This image of his left ear was obtained with the Wispr.
The child has acute otitis media with a hemorrhagic bulla.
The image shows all the classic features of acute otitis media. These features include bulging of the eardrum, erythema, and loss of bony landmarks. The lateral process of the malleus is barely discernable.
What’s interesting in this image is the dark area in the middle. This appears like bullous myringitis which is blistering of the tympanic membrane from infection. In this case, the central blistering likely occurred over a superficial capillary of the tympanic membrane causing a blood-filled or hemorrhagic bulla.
Treatment of this condition is the same as acute otitis media or bullous myringitis. A course of standard antibiotics along with analgesia with ibuprofen and acetaminophen. Careful return precautions should be given to the family in the event of worsening symptoms despite treatment.
Here is the complete video exam of the child’s left ear:
Complete video of exam

Otitis Externa
A 9-year-old female with ear pain is brought into the emergency department by her mother. The family is from out-of-town and is visiting relatives on holiday. The mother is an emergency physician in her hometown. She reports that her daughter has been doing a lot of swimming while on vacation and that about two days ago she began to develop right ear pain. The physician-mother reports examining the ear and felt her daughter most likely had otitis externa based on history and exam. She placed her daughter on systemic and drop antibiotic therapy. The child has had no improvement in symptoms and was brought to the local emergency department for evaluation. The following image of the right ear was obtained.
The child has otitis externa (swimmer’s ear), an infection of the external auditory canal.
This is a typical presentation of otitis externa. Ear pain and discharge that develops after swimming. It is thought that excess exposure to water causes breakdown of the skin in the ear canal offering bacteria the chance to overcome the normal cerumen defense factors. The external canal will normally be swollen with the canal appearing red, painful to inspection, and often times (as in this case), obstructed by purulent discharge. Treatment is antibiotic drops. Although the patient had been on antibiotic drops, it was not a first-line antibiotic. In addition, the physician-mother did not have ear wicks available. The use of ear wicks is indicated as the antibiotic drops have to penetrate the edematous canal to reach the distal areas of the external canal.
The child was placed on a first-line antibiotic and was provided with ear wicks.
Here is a video of the ear exam:
Complete video of exam

Middle Ear Effusion
A 32-year-old woman presents to the emergency department complaining of left ear pain. She reports having the pain for about one week. She was seen in the clinic a week ago, diagnosed with left acute otitis media, and placed on an oral antibiotic and antibiotic drop, both of which she has completed. She reports no improvement in pain and describes a fullness in her left ear. Prior to the ear pain starting a week ago, she had mild viral symptoms including congestion and a runny nose. She tested negative for COVID-19. A colleague examined the patient with a traditional analog otoscope and thought the patient likely has unresolved otitis media and that the ear looked “red.” He asks for your input using the Wispr digital otoscope. What is your recommendation to the colleague?
The patient has a middle ear effusion (MEE).
Compare the left ear MEE to the normal right ear.
This is a common clinical scenario. Unresolved ear pain after a course of antibiotics prescribed for acute otitis media (AOM). In this case, the patient does not have acute otitis media. The Wispr image clearly shows a non-bulging tympanic membrane (eardrum) with normal malleus bony landmark. In addition, there are air-fluid levels surrounding the malleus, a clear indication of middle ear effusion.

The air bubbles indicate the middle ear space is being ventilated by the eustachian tube. There is no indication for prescribing another course of antibiotics. The patient was shown both the image of the left ear with MEE and her normal right ear. She was reassured by being able to see the images herself and no further discussion of antibiotics was necessary.
Here are the videos from both the left and right ear exams.
|
Left Ear Video |
Right Ear Video |
Additional information on normal, MEE, and AOM can be found here.

Malleus and Components
Otoscopic examination of a healthy 57-year-old male reveals this image.
Can you identify the malleus and its components?

The malleus (commonly called the “hammer”) is the first bone in a chain of three middle-ear bones that translate movement of the tympanic membrane to the inner ear. The malleus is the most prominent landmark visible in the middle ear space. The malleus is also an anatomical compass in that it “points” to the face. This allows you to determine that this is the left ear.
The portions of the malleus that are visible on otoscopic examination include the umbo, manubrium, and the short process. The short process is often the last portion of the malleus that is discernable in cases of infection as in this example. All of these portions are attached to the tympanic membrane (eardrum). As the tympanic membrane vibrates from sound waves, the malleus converts this vibration into a rotary motion at the head (not visible) that is connected to the incus and then to the stapes.
Here is the complete video exam:
Complete exam video

Pulsatile Tympanic Membrane Perforation with Effusion
A previously healthy 9-year-old male presents to the pediatric clinic with two days of left ear pain and ear drainage. The child reports intermittent and improving drainage. On review of systems, the child has had no cough, no congestion, and no fevers. Physical exam was unremarkable except for a pulsating finding in the left ear.
This is well-visualized on the video:
The child has a pulsatile tympanic membrane perforation with effusion.

The tympanic membrane (TM, ear drum) is clear not normal. There are changes to the TM that are consistent with the medical history of ventilation tubes including myringosclerosis. The malleus ossicle, while discernable, is not clearly defined. Most dramatic, is the small defect in the TM with an unusual pulsation.
The patient was referred to ENT who was only able to see profuse otorrhea and treated the child for otitis externa. However, ENT was able to review this video obtained from the primary care pediatrician. The differential diagnosis included vascular tumor vs middle ear effusion communicating vascular pulsation. Looking at the pulsation on the video, the rate of pulsation (about 96 pulses/minute) appears consistent with the heart rate of a 9-year-old patient.
This case illustrates the dual benefits of the Wispr. First, the ability to record video, and second, the ability to share that record with specialists.

Bullous Myringitis
A five-year-old male child presents to the ED with ear pain and fever. His mother explains that the child’s symptoms started with a runny nose about 4 days ago. He then developed a cough and congestion. About a day ago, the child complained of ear pain and fever to 102.1 F. The mother has been treating with fluids, acetaminophen, and ibuprofen. Treatment transiently helps with the symptoms and provides comfort. The child’s older siblings had viral symptoms that resolved about a week ago. The child continues to eat and drink, but with less enthusiasm. A chest x-ray does not show pneumonia, and a rapid strep test comes back negative. This image of the child’s ear is obtained.
The child certainly has acute otitis media (AOM) and likely bullous myringitis.
Acute otitis media (AOM) is an infection in the middle ear space. This is the space behind the tympanic membrane. The infection causes inflammation that causes the eustachian tube (middle ear drainage channel) to become closed. The closed eustachian tube combined with inflammation causes fluid build-up in the middle ear. This causes bulging of the eardrum and is quite uncomfortable. Bullous myringitis may be considered to be a severe form of AOM where there is blistering on the tympanic membrane. In this case, there does appear to be blistering developing in the central part of the tympanic membrane, the pars tensa. Bulging along the periphery of the membrane is clearly visible, consistent with AOM. The blistering of the tympanic membrane can result in a hemorrhagic bulla as in this example.
Compare the images below. A normal ear, acute otitis media (bulging), and bullous myringitis (bulging with blistering).
Treatment is focused on providing pain relief along with treating the underlying infection. An anesthetic such as topical lidocaine can be introduced in the ear canal to provide timely pain relief. Treatment of the underlying infection is the same as for acute otitis media. For children that have frequent cases of AOM, ventilation tubes may be indicated.

Middle Ear Effusion
An 8-year-old female with a history of ear infections presents to the pediatric clinic for a well-child check. She has had mild cold-like symptoms including rhinorrhea and congestion. She does not have a fever, and she does not complain of ear pain. She continues to eat and drink well and be active. Examination of the right ear reveals this image.
The child has a middle ear effusion (MEE).
This is a common clinical scenario. A previously well child with mild viral symptoms. The ear shows air-fluid levels consistent with a middle ear effusion (MEE, fluid in the middle ear space, behind the tympanic membrane). The air-fluid levels in the image are at the 6 o’clock position. In reality, because of the way the Wispr otoscope is being held, the air-fluid levels are anatomically in the anterior-superior region. The presence of air along with fluid in the middle ear space suggests that the eustachian tube is functioning properly. Because the eustachian tube is functioning properly to equalize the pressure on both sides of the eardrum, there is no bulging as would be seen in acute otitis media (AOM). In addition, there is no indication for intervention such as antibiotics. The fluid will drain through the eustachian tube with time.
Compare the following images of eardrums: normal, middle ear effusion, and acute otitis media. You can clearly appreciate the difference between the MEE with a functioning eustachian tube and the AOM with profound bulging indicating a non-functioning eustachian tube.

Foreign Body
A 6-year-old male is at the pediatric clinic for a routine child exam. The child has no complaints and his mother has no concerns. Examination of the ears reveals this image.
The child has a foreign body in his ear.
After seeing the foreign body, the mother mentioned that the child was playing with a friend in the sandbox. The foreign body was easily removed with a curette. Upon removal, it appeared that it might be a bead or tiny pebble.
Amazing what ends up in kid’s ears!
WiscMed thanks Dr. Thomas Schreiner of the Indian Health Service for this case.

Acute Otitis Media
An 8-year-old male arrives with his mother at the emergency department complaining of left ear pain. The pain started 4 days ago and has become worse. The child had ear infections as a toddler, but none recently. In addition to the ear pain, for the past several days he has also had seasonal allergy symptoms including watery eyes and a runny nose. Evaluation of the left ear reveals this image.
The child has acute otitis media (AOM) of the left ear.
There is a significant bulging of the pars flaccida, loss of the malleus bony landmark, and erythema (redness). Given the history of worsening pain, along with this imaging, the child was placed on a course of antibiotics.
Compare the left ear with the right ear:
The right ear has some erythema, along with mild bulging of the pars flaccida. The malleus is still discernable. This ear alone would not have been an indication to start antibiotics.
Here are the video exams of both ears. You can appreciate how well the Wispr otoscope is able to maneuver around the cerumen present in the canal.
|
Left Ear Video |
Right Ear Video |
Here are links to two other cases featuring acute otitis media (AOM). AOM 1 and AOM 2.

Tympanic Membrane Defect with Middle Ear Discharge
A 15-year-old male presents to the pediatric clinic with ear discharge. The patient has had a history of two tympanoplasties by ENT. He does not have any ear pain. He does have decreased hearing. What is your diagnosis?
This patient has Tympanic membrane defect with Middle ear discharge.
The patient has a chronic appearing tympanic membrane defect. In addition, when the patient does the Valsalva maneuver, fluid draining from the middle ear space is clearly seen.
This is well-visualized on the video:
It is not clear the nature of the fluid, but an infection was suspected. The patient was placed on antibiotic drops and referred to ENT.
WiscMed thanks Dr. Jack Whitehead of Brentwood Children’s Clinic of Brentwood, Tennessee for this interesting case.

What is Your Advice?
A medical student is rotating in the pediatric clinic. She shows her attending the following three ear images. She wants to start antibiotics on all three patients.
Do you agree that antibiotics should be started?
Besides its ability to obtain reliably diagnostic images of the tympanic membrane, the Wispr digital otoscope is also good for sharing images with learners, patients, and families. These three images demonstrate commonly observed otoscopic findings.
Myringosclerosis

Sclerosis
The first image is of myringosclerosis (sclerosis). This is localized thickening (calcification) of the eardrum, generally observed to be white, as in this case. The sclerosis is generally from an eardrum that has been damaged and then healed. Common causes of damage include tympanostomy (ventilation, ear) tubes and traumatic rupture of the eardrum. Sclerosis, although often dramatic, does not generally materially affect hearing. Sclerosis is not an indication to start antibiotics. It represents a well-healed eardrum and no further intervention is necessary.
Tympanostomy (Ventilation, Ear) Tubes
Ventilation Tubes
The second image shows a well-positioned tympanostomy tube (blue circle) in the anterior-inferior portion of the pars tensa tympanic membrane. There is a minor amount of debris around the annulus of the tube that might be cerumen (ear wax) or it could be drained and congealed middle-ear fluid. The rest of the eardrum is completely normal with a pearly grey light reflex, concave surface and the malleus bone clearly visible.
Ventilation tubes are inserted to drain the middle ear space. They are generally placed in children who have recurrent acute otitis media (AOM). The tubes fall out on their own in months to years. After the ear tube falls out, there is generally an area of sclerosis present as above. A ventilation tube in an otherwise normal-appearing ear is not an indication to start antibiotics.
Acute Otitis Media (AOM)

Acute Otitis Media
The third image shows a mild case of acute otitis media. There is bulging of the pars flaccida and the superior-posterior portion of the pars tensa tympanic membrane. There is a partial loss of the malleus bony landmark. This case appears to be mild because the bulging is not severe in the inferior portion of the tympanic membrane. The decision to start antibiotics, in this case, is indeterminate. It would depend on how ill the child is and how long he has had the symptoms. Of the three images presented, this is the only case where antibiotics should be considered.

Hair in View
A 54-year-old man presents to the emergency department for a complaint of dental pain. As part of the exam, this image of an ear was obtained.
What is the bright line on the image?
The patient has an ear hair that is seen in this image.
The ear canal is a surprisingly complex piece of human anatomy. The tympanic membrane (eardrum) is located at the very end of the ear canal, about 1 cm deep to the ear opening. In addition, the canal is not a straight tube, there is a bend. Further complicating matters are natural obstructions in the canal including hairs and cerumen (wax). In this image, the bright white vertical line is light reflected off of a hair. You can also see dry cerumen layering inferiorly near the tympanic membrane.
Because examination of the ear canal has many challenges, being able to capture a video of the exam is very helpful. Here is the video of the exam from which the image was exported. The video allows you to see the entire canal and eardrum improving your ability to determine the context of what you are seeing.
Complete video of exam
Bonus questions, which ear is this, and can you find the incus bone and the chorda tympani nerve?

Acute Otitis Media
An 18-month-old female is brought into the pediatric clinic by Dad with fever and fussiness. About 3 days ago, the child developed a cough and runny nose. Today, she had a temperature of 39 C at home. She has been receiving acetaminophen and ibuprofen for her symptoms. The medication helps with the fever for a few hours. She continues to eat and drink, but without much enthusiasm. She has frequent wet diapers. On exam, she is a well-nourished infant. She appears ill but not toxic. She appropriately resists the exam and is easily comforted in her Dad’s arms. A urinalysis came back negative. The above image of her left ear was obtained.
The child has acute otitis media in her left ear.
This is a classic presentation of acute otitis media (AOM). The tympanic membrane is bulging with marked erythema and pronounced vasculature. The bulging is due to increased pressure in the middle-ear space. This image is a beautiful example of AOM in that the bulging is not complete in the anterior-inferior pars tensa. In addition, it’s still possible to make out the lateral process of the malleus. It would be appropriate to start antibiotics on this patient. Compare the left ear with AOM to the normal right ear. The right ear has some erythema, but no bulging and the malleus is clearly visible.

Initiate Antibiotics?
Presentation
A five-year-old is brought to the pediatric clinic by his mother with concern for fever. The mother reports that the child has had a cough, runny nose, and temperature at home to 101 F. He is vaccinated. He continues to eat and drink, but with less enthusiasm. He is irritable and sleeping more than normal. She reports a history of ear infections. She has been treating the child with Tylenol. The child cries during the exam with copious tears and a normal posterior pharynx. He has a brisk capillary refill. His lungs are clear and he is mildly tachycardic for age. He is easily comforted by the mother. Examination of the left ear reveals the above image.
Discussion
This a very common presentation in the primary care clinic, a fussy child with a mild temperature. There are a number of decisions that need to be made. The first decision is the likely cause of the symptoms. Most important is to rule out a life-threatening cause like meningitis. In this case, the symptoms of cough and rhinorrhea with clear lungs and a mild fever suggest a benign viral respiratory infection. It’s reassuring that he is well-hydrated and fussy yet consolable by the mother. The second decision is if medical intervention is necessary. In this case, the child’s lungs are clear suggesting no pneumonia. The image of his ear shows increased vasculature and erythema consistent with crying. This is a good example of an ear presentation that could be mistaken for acute otitis media if you just had a very quick glimpse of the ear. However, with the Wispr digital otoscope, it is clear that there is no bulging of the ear drum, no effusion, and the malleus bony landmark is intact. There is clearly no indication for antibiotics. Treatment is analgesia such as acetaminophen or ibuprofen along with comfort care.
Compare the normal ear in this case (no treatment required) to a case of acute otitis media (antibiotic indicated).

Worried Parents
Parents of a 16-month-old present to the University of Wisconsin – Madison academic Emergency Department with their child for a second opinion. They report that their son has been pulling at his ears frequently over the past month and occasionally seems uncomfortable. They have not recorded a fever and he has not been congested or otherwise ill. They took him to the local ED three weeks ago where he was diagnosed with an ear infection and prescribed an antibiotic for 10 days. The patient completed the antibiotics but they did not notice any improvement—he was still occasionally irritable and sticking his fingers in his ears—so they had him follow-up with his primary physician who described “fluid behind his ears.” Unsatisfied, the parents then decided to drive 60 miles to our Pediatric Emergency Department for another assessment.
The following images were obtained with the Wispr:
What is your diagnosis and action plan?
The child’s Wispr exam revealed very normal-appearing tympanic membranes without evidence of bulging or middle ear effusion (MEE). In fact, recalling that it can take 4-6 weeks for full resolution of MEE and normalization of the TM appearance, the findings made us question (internally) the recent diagnosis of an otitis media requiring antibiotics. Regardless of whether or not he indeed had rapid resolution of an AOM, the child does not have evidence of MEE as reported earlier today.
What to do about a fussy 16month-old who is constantly “pulling at his ears”? Toddlers obviously pull at their ears for any number of reasons that are unrelated to AOM or MEE. From the impressive-sounding Eustachian tube dysfunction to the simple fact that little kids sometimes pull at their ears just because they are there, providers must caution that they do not default to AOM nor dismiss parental concerns by reporting questionable physical findings. As can be learned from this case, such an approach may result in unnecessary anxiety, inconvenience, and medical costs–by a reasonable estimate, the total healthcare expenses of this episode easily surpassed $1000.
One of the most obvious benefits of utilizing digital otoscopy is ensuring an accurate diagnosis. However, a close second is the ability to share the objective findings with your patients and parents. As we reviewed their child’s Wispr exam, I took the exact same approach that I use when teaching; pointing out landmarks, lack of bulging, redness, or fluid. During this review, I also pointed out a finding that all of you have surely already identified—there is a small dark brown hair up against the child’s left TM. The parents note that they have a black lab (awesome dogs, but notorious for shedding). While the family pet is likely the source of the little hair, whether this is actually the reason for the child to pull at his ears is unclear. It seems rational, but I would not discount the fact that the child just likes to pull on his ears. Regardless, the parents left the ED feeling very relieved, satisfied, and confident that nothing worrisome was being missed.
Here are videos of the exam from each ear:
|
Left TM |
Right TM |

Perforation of the Tympanic Membrane
A 65-year-old woman presents to the emergency department complaining of left leg weakness. She has had multiple falls today. She has been feeling “dizzy” and her left ear has been “popping.” Her son accompanies her and also says that her speech is not normal. She has a history of smoking for many years. This image of her left ear is obtained.
The patient has a perforation of the tympanic membrane in the anterior pars tensa.
The perforation looks chronic and is likely not related to her presentation tonight. The perforation extends to the anterior surface of the malleus. The eustachian tube orifice is seen through the defect in the tympanic membrane. Surprisingly, the patient does not complain of decreased hearing in this ear.

Here is the video of the patient’s ear exam:
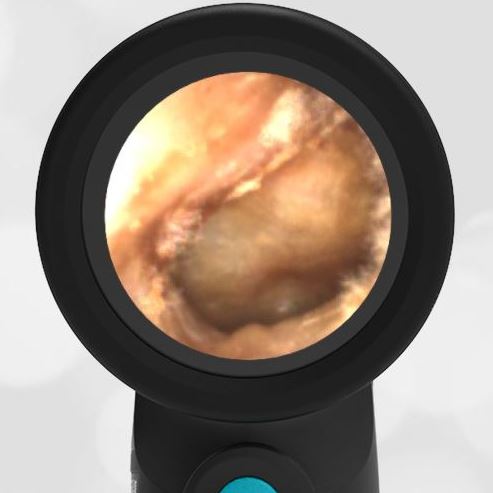
Otitis Media
An 82-year-old male seeks medical care for ear pain. Two days prior he reports left upper jaw pain that radiated to his left ear. The pain subsequently localized to his left ear. He describes the pain as a baseline throbbing with an occasional sharp component. He reports dental care about 2 weeks ago. No history of fevers, difficulty swallowing, difficulty breathing, facial swelling, or changes in hearing. The patient noticed increased ear discomfort during a recent airplane trip. He reports that sweets bother his teeth. On exam, he is a well-appearing male appearing younger than the stated age. He is chatting comfortably with no noted hearing problems. He walks with a steady gait. Axial loads of teeth 14 and 15 do not elicit any discomfort. No acute dental deficits are noted. Visualization of the left ear was heavily comprised by cerumen, however this image of the right ear was obtained.
This patient has Otitis Media.
Although visualization of the left ear in question was incomplete, there was evidence of loss of definition of the malleus at the pars flaccida. This could be associated with acute otitis media. The right ear was better visualized and has a donut appearance consistent with fluid collection in the middle ear space. There is no distinct erythema associated with the tympanic membrane suggesting that this may be a chronic condition.
This is a typical clinical scenario with associated diagnostic uncertainty. Given the history of recent dental cleaning along with the origin of the discomfort being at the upper left jaw with subsequent migration to the ear, it seems reasonable to conclude that a mild bacterial infection could be the cause of the patient’s symptoms. It is unclear if the finding of the right ear was chronic or acute. The patient reported poor baseline hearing from the right ear. The patient was allergic to primary antibiotics and so was placed on a course of a secondary antibiotic. During follow-up with the patient over the next two days, he reported complete resolution of symptoms.
Here is the video of the patient’s right ear exam:

Foreign Body – Spider in Ear
A 5-year-old male presents to the pediatric clinic complaining of tickling and noise in his right ear.
The child has a spider in his ear canal.
The image shows a spider in the child’s ear. 2 ml of topical 1% xylocaine was instilled in the ear and allowed to dwell for 5 minutes. The ear was then irrigated and the spider was uneventfully flushed.

Foreign Body – Spider

Chorda Tympani Nerve
A 27-year-old female medical student is on her emergency medicine rotation. She is learning ear anatomy. The following image of her left ear is obtained.
Can you help her identify the chorda tympani nerve?
 |
Chorda Tympani Nerve Chorda Tympani Nerve Video
The chorda tympani nerve traverses medial to (“behind”) the malleus and lateral to (“in front of”) the incus. In this image the chorda tympani is visible behind a highly translucent tympanic membrane:

Chorda Tympani Nerve
Surprisingly, the function of this nerve has nothing to do with the ear, it simply traverses the middle ear space where on occasion it can be seen behind a transparent eardrum, as in this case. The nerve is a branch of the facial nerve and provides sensation to the anterior two-thirds of the tongue. It also provides parasympathetic fibers that provide motor innervation to the submandibular and sublingual glands.
Here is a second example of the chorda tympani nerve from a 10-year-old female:

Chorda Tympani Nerve – 10-year-old female

Normal Left Ear Drum
A healthy 62-year-old woman presents for a routine physical exam. This image is obtained of her left ear.
Can you identify at least 5 of the following features of this normal ear?
- Ear Canal
- Tympanic Membrane
- Cone of Light
- Pars Tensa
- Pars Flaccida
- Eustachian Tube Shadow
- Malleus Bone
- Incus Bone
- Stapes Bone
- Chorda Tympani Nerve




More information and background is found in this Wispr University article, Normal Ear Anatomy as Seen by Otoscopy.

Otoscope Grip Preference
A pediatrician shows a Wispr otoscope image to their emergency physician colleague. The emergency physician is initially confused by the image.
Why does the image initially seem confusing to the emergency physician?
The pediatrician is holding the otoscope differently.
Generally speaking, the otoscope orientation that pediatricians use is 180 degrees different from non-pediatric physicians. The orientation of the saved image is dependent on the orientation in which the otoscope was held. These exam photos demonstrate the difference in the resulting ear image. The image is rotated 180 degrees corresponding to the grip used on the digital Wispr otoscope.
Once the orientation of the otoscope is taken into account, it is a simple matter to mentally rotate the image such that the malleus always points “upward.” Pediatricians are trained to use the superior orientation of the otoscope as it is thought to give better control in the case of a squirmy patient. In both orientations, the examiner should stabilize the otoscope position with fingers such that a sudden movement of the patient’s head does not cause undesired movement of the otoscope.
Here are videos of the two otoscopy techniques:
|
Pediatric Grip |
Alternate Grip |

Perforation of the Tympanic Membrane
A 55-year-old male with chronic right ear discharge and hearing loss presents for evaluation at the ENT clinic. He has a history of recurrent acute otitis media treated with multiple courses of antibiotics. He has had ventilation tubes in the past. This image is obtained.
The patient has a perforation of the tympanic membrane.
You can clearly see the defect in the tympanic membrane (TM, eardrum), it is the circular area on the left-middle of the image. This is anatomically the inferior portion of the TM, located in the pars tensa. The malleus is also clearly visible extending from the center of the image to about the 5 O’clock position. The defect is likely due to the history of ventilation tubes and poor healing of the TM. In addition, the patient has myringosclerosis. This is the white area at the bottom of the image.
Here is the video exam of this patient:
WiscMed thanks Dr. Todd Morrow of Associates in Otolaryngology, West Orange, NJ for this interesting case.

Otitis Media with Effusion
A healthy 3-year-old male with one day of rhinorrhea and cough is in for COVID testing after a school exposure. The child apparently had similar symptoms several weeks prior that resolved spontaneously. The child’s COVID test was negative.
The child has otitis media with effusion.
You can see fluid layering inferiorly behind the tympanic membrane. There is also evidence of mild bulging, but the malleus is still discernable. The family was asked to return the next day in follow up to make sure of resolution.
At the second visit, this image was obtained:

In this image, the bulging appears to be mildly improved. The inferior layering of fluid is resolving into air-fluid levels. This suggests that the eustachian tube is properly venting and that the middle ear effusion will resolve without intervention.
WiscMed thanks Dr. Caroline Rowlands of Optum Care Colorado Springs for this interesting image.
WiscMed thanks Dr. Michael Poole of Savannah Pediatric Ear, Nose and Throat for his consultation on this case. His book, Acute Otitis Media, is available on Apple books and is highly recommended.

Pars Tensa and Pars Flaccida
A 25 year old medical student is on her internal medicine rotation. She has questions about ear anatomy after examining her 11 AM patient. She obtained this image using the Wispr otoscope and would like to understand the difference between the pars tensa and the pars flaccida portions of the tympanic membrane.
There are two distinct areas to the tympanic membrane (eardrum), the pars flaccida and the pars tensa.
These two areas are outlined in the following images:

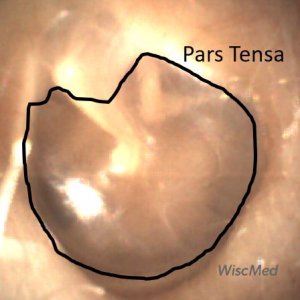
The pars tensa is the portion of the tympanic membrane that is the largest. It’s what people tend to think of when they think of the “eardrum.” As the name suggests, it is “taut,” much like if you stretched plastic wrap on top of a bowl. You could also imagine the pars tensa to be similar to a drum surface. It is the portion of the eardrum responsible for translating sound waves into mechanical movement.
The pars flaccida, as the name suggests, is less “taut” and also thicker. It drapes across the superior portion of the malleus. Although it does not have an active role in sound wave transcription, it is necessary to provide complete coverage of the middle ear space and allow for the proper functioning of the pars tensa.
From a clinical perspective, the pars tensa gets most of our attention. This is the place where we would expect to see perforations, effusions, and the characteristic bulging of acute otitis media.
The pars flaccida may be the first place that bulging of the tympanic membrane is seen due to increased pressure in the middle ear space. The pars flaccida is where most eardrum movement would be appreciated if evaluating mobility of the eardrum via either pneumatic otoscopy or a Valsalva maneuver.
Bonus: Which ear is this? It is the left ear.

Eustachian Tube Dysfunction
A 53-year-old woman complains of mild discomfort in her right ear and a sensation that her ear is “clogged.” She compares it to the discomfort during an airplane in descent before the ear “pops.” She otherwise feels well. No cough, rhinorrhea, fever, sore throat, or weight loss. She does not have vertigo. She has not tried any medications for the symptoms.
The patient has eustachian tube dysfunction.
This diagnosis is not evident by the image alone. The image shows a pearly grey eardrum, normal bony landmarks, and a normal light reflex. The patient was asked to perform a Valsalva maneuver during which the following video was obtained:
Prior to treatment – no movement of the ear drum when patient performs Valsalva
In this video, there is no movement of the eardrum when the patient increases the middle ear pressure with the Valsalva maneuver. This suggests that pressure across the eardrum is not being properly equalized by the eustachian tube. This is known as eustachian tube dysfunction and can be quite uncomfortable. The eustachian tube vents the middle ear to the back of the nose. For most of its course, it’s like a floppy, hollow noodle. It can become inflamed, causing it to be “sticky” and limiting its ability to properly vent the middle ear space. A difference in pressure across the eardrum causes the familiar feeling of discomfort in an airplane in descent. More information on ear anatomy can be found on this Wispr University article.
Eustachian tube dysfunction can occur for a number of reasons including allergies, infection, and irritants. Less likely causes would be anatomical changes associated with trauma or lesions. Initial treatment in the primary care clinic could include decongestants or steroids. Evidence for the effectiveness of treatment is not strong. If the patient continues to have symptoms, they should be referred to otolaryngology.
In this case, the patient was trialed on a nasal decongestant. On re-evaluation, the patient reported improved comfort and a repeat video exam showed mobility of the tympanic membrane at the pars flaccida.
You can see this as the increase in the brightness as the top of the eardrum moves:
After nasal decongestant – movement of pars flaccida with Valsalva
Use of a nasal decongestant is not recommended for more than a few days. When the patient discontinued use, her symptoms returned. She was referred to otolaryngology.

Cartilage Lesion
A 27-year-old female with a history of metabolic syndrome and cholesteatomas presents to the emergency department with a complaint of chest pain. During the physical examination, she is noted to have a bone-anchored hearing aid (BAHA) posterior-superior to her right ear lobe. Further questioning elicits that she has a history of multiple ear surgeries and has significantly diminished hearing in each ear. This image is obtained of her left ear.
The patient has a cartilage lesion.
The patient has a lesion superior to her malleus. In addition, she has changes to the tympanic membrane including sclerosis. that support her history of ear surgeries. The patient relates that as a child she had cholesteatomas in each ear requiring surgery. Cholesteatomas are often the result of the eustachian tube dysfunction allowing for the accumulation of keratin in the middle ear space. This accumulation can damage both the eardrum and the chain of bones. When this occurs, surgery is required to repair the structures. The lesion seen in this image is most likely cartilage secondary to that repair.
Here is a video of the left ear:
The patient had similar changes to her right ear.
WiscMed thanks Dr. Michael Poole of Georgia Ear, Nose and Throat for consulting on this case and we highly recommend his book “Otitis Media” available currently at no charge on Apple Books.

Desquamated Keratin
A 53-year-old woman complains of right-sided ear pain with radiation down her jaw. She thinks the pain is associated with recent migraines she has been having. No change in hearing, no tinnitus or vertigo. She does not have any history of ear trouble. She has not had any fevers, nausea, or vomiting.
The patient has desquamated keratin or sloughing of a large number of skin cells.
It is easy to mistake desquamated keratin for cerumen (ear wax). This image nicely demonstrates both cerumen, which is in the lower-left portion of the image with desquamated keratin, which is in the upper-right. The cerumen is a globular, sticky substance while the keratin is a sheet-like, folded substance. Cerumen is a normal finding in a healthy ear. Large amounts of desquamated keratin are not seen in a healthy ear. It suggests that something has irritated the ear canal causing sloughing of the skin. In severe cases, this sloughing of the skin can be so extreme that it causes a painful and solid blockage of the ear canal known as keratosis obliterans.
Here is a video of the ear canal:
The keratin and the cerumen were removed with a combination of curette and irrigation.
Here are side-by-side images of the canal before and after removal:
It’s apparent that the patient has several areas of irritation to the external auditory canal. An antibiotic ear drop with a steroid was prescribed.
Follow up pictures were obtained that nicely demonstrate resolution of the inflammation of the ear canal:

Middle Ear Effusion
A 3-year-old with a history of chronic middle ear effusion is brought in by her mother to the pediatric clinic with concern for ear discomfort. This image is obtained. What is your diagnosis?
The child has a middle ear effusion.
A significant challenge in otoscopy is seeing the difference between acute otitis media (AOM) and a middle ear effusion (MEE). The key point of differentiation is the presence of bulging of the eardrum. Bulging indicates increased pressure in the middle ear space and is the hallmark of AOM. In this clinical case, there is no bulging, but there are clearly air-fluid levels consistent with MEE. In addition, the eardrum does not look “angry”, i.e. it is not erythematous and the vasculature is not prominent. For this case, no treatment is indicated. Compare this with bullous myringitis, a significant infection that results in blistering of the eardrum.
The attending physician reports that the mother didn’t initially understand the meaning of a middle ear effusion. However, when the mother was shown this picture, they were able to have a reassuring discussion of MEE and why it did not require treatment.
WiscMed thanks Dr. Kate Robinson of Lyndon Pediatrics, Fayetteville, NY for this interesting case.

Foreign body – bead in ear
A previously healthy 9-year-old male presented to the emergency department with concern for a foreign body in his right ear. Earlier, he was playing with plastic necklace beads on a trampoline when the family dog joined him (what can go wrong from here, right?).
The child has a bead in his ear canal.
Otolaryngology (ENT) was consulted due to concern that the bead was close to the tympanic membrane (TM, eardrum), and the risk of TM damage during removal. An alligator forceps (from a myringotomy set) with visualization from the Wispr otoscope was used to uneventfully remove the bead.
WiscMed thanks Dr. George Liu of Stanford University School of Medicine – Otolaryngology for this interesting case.

Complete ear wax (cerumen) obstruction
A healthy 50-year-old female complains of marked decreased hearing in her left ear. She has no pain and does not report a history of trauma although she is an avid swimmer. She has a history of significant ear wax and believes this may be the problem. She tried an over-the-counter ear drop to remove the wax, but her hearing did not improve.
The patient has complete obstruction of her left ear canal with ear wax (medical term, cerumen).
Individuals can have very different ear wax properties, from scant production to copious. Ear wax can also vary from hard to soft. Generally, the younger the patient, the softer the ear wax.
Here are videos of the ear before and after wax removal:
The wax was easily removed with a speculum and a curette.
The patient reported an immediate improvement in hearing after the wax removal.

Prominent Vasculature
A tolerant spouse of a WiscMed staff member submitted to yet another ear exam. She has no prior history of ear trouble and no complaints of decreased hearing. She reports feeling well. What do you notice about this image that was obtained of her left ear?
The image of the ear shows prominent vasculature (blood supply).
This is especially noticeable on the malleus, but also on the ear canal and to some extent on the tympanic membrane (eardrum). The cause of this is unclear. Possible explanations could include mild trauma, inflammation, hydration status, body temperature, recent body position (supine vs upright), elevated blood pressure, and medications that dilate vasculature. In this case, none of these explanations seems plausible and we are left wondering about the cause.
A repeat image of the same ear taken the next day, 12 hours later, shows resolution. There does not appear to be any clinical significance to the transient prominent vasculature.
At WiscMed University you can find the article on “Normal Ear Anatomy as Seen by Otoscopy“.

Do you agree with the diagnosis of acute otitis media?
A 20-month-old male presented to the emergency department with a fever and rash. The child was seen in urgent care the previous morning for the same complaints and diagnosed with “bilateral ear infections.” He was started on the usual antibiotic and had taken three doses. Mom reported that the child continued to have a fever and was fussier, so she brought him to the Emergency Department (ED) for re-evaluation. Upon further questioning, she stated her child had a fever up to 103 F each of the prior five days. Also, she noted the appearance of a diffuse non-itchy rash yesterday.
The physical examination was significant for a nontoxic but irritable toddler. An exam with the Wispr Digital Otoscope was performed and pictured below. The remainder of the HEENT assessment revealed bilateral non-purulent conjunctivitis with limbic sparing. He had a morbilliform rash on the trunk and extremities. Both hands and feet were slightly swollen and tender.
The tympanic membranes (TMs) are normal with no evidence of erythema, bulging, loss of bony landmarks or middle ear effusion. This is not consistent with acute otitis media (AOM).
Clearly, the source of fever for this child was not acute otitis media (AOM) and demonstrates, once again, the importance of an accurate ear exam in the febrile child. In this particular case, the misdiagnosis could have had potentially severe consequences since the child presented to the ED with signs and symptoms of a more worrisome condition as the true etiology of his fever. With the constellation of five days of fever, bilateral conjunctivitis, swollen hands and feet, rash, and elevated inflammatory markers, the differential diagnosis included incomplete Kawasaki Syndrome (KS). Also, given the current public health crisis, Multi-System Inflammatory Syndrome in Children (MIS-C) which has overlapping features with KS was entertained. Thus work-up in the ED included SARS-COV-2 PCR which was negative. However, his IgG antibodies to the virus were positive, indicating past exposure and elevating MIS-C as the likely etiology of his illness. He was found to have additional systems involved with elevated B-natriuretic peptide and mildly dilated coronary arteries indicating cardiac involvement as well as increased d-dimer and fibrinogen consistent with the highly inflammatory state (and potential hypercoagulable state) observed in COVID infections.
Current management for incomplete KS and MIS-C are similar and the child was admitted and treated with IVIG and aspirin. Over the course of four days, he improved clinically with no fever and down-trending inflammatory labs. He was discharged home in good condition with appropriate follow-up arranged with multiple subspecialties.
Additional Discussion from attending physician Dr. Greg Rebella:
This is an interesting and timely case given the COVID-19 pandemic (November 2020). It also provides the opportunity to highlight a couple of important points pertinent to the ear exam. The first point is that we have all found ourselves in a situation where an examination of the tympanic membranes (TMs) is suboptimal and thus our assessment likely to be less accurate. Perhaps we might even have been biased toward AOM because we have not found any other source of the fever. Thus, it is not surprising that without a clear view of the TMs clinicians might fall into the trap of over-calling mild or nonexistent findings as otitis media. This is likely what occurred in the present case. This 20-month-old was fussy, anxious, and not in a mood to allow any more than a few seconds to look at his TMs. Fortunately, with the Wispr Digital Otoscope this is all that is needed (5 seconds for the right TM, 6 seconds for the left – see videos below). And once images of the TMs are digitally captured, we can step back and closely analyze them for physical indicators of pathology while the child sits comfortably in his mom’s lap.
The second point of discussion was the question of whether or not the child could indeed have had TM changes consistent with AOM, and that our current findings represented a clinical improvement. In other words, how quickly can TMs return to normal after initiating antibiotics? The answer to this question is that the development of AOM is a continuum with the development of middle ear effusion (MEE), progression to acute otitis media, and resolution with the persistence of MEE for a period of time. Given the lack of MEE on our Wispr exam, it seems highly unlikely that one day prior there had been an infected MEE consistent with AOM.
WiscMed thanks Dr. Greg Rebella of the BerbeeWalsh Department of Emergency Medicine and of WiscMed for this interesting case.

Acute Otitis Media (AOM)
A 4-year-old female with a history of ear infections presents to the pediatric clinic with 3 days of rhinorrhea, malaise, and temperature to 102.3 F. Several hours ago, the child began to complain of right ear pain. The mother has been treating the child with Tylenol. The following image is obtained from the right ear.
The child has acute otitis media (AOM).
You can also see a clear air-fluid level behind the tympanic membrane in the superior-anterior (right-upper) location. The key diagnostic feature of AOM is a bulging tympanic membrane as seen in this image. As also seen in this image, there is often a loss of the malleus bony landmark and of the cone of light. Erythema (redness) is usually present. This may be an early presentation of AOM as the malleus bone is still partially recognizable. Compare this presentation to otitis media with effusion (OME). Both have air-fluid levels and some erythema. The difference between AOM and OME is the bulging of the tympanic membrane. AOM is usually treated with antibiotics while OME is observed. The air-fluid level is caused by fluid behind the tympanic membrane that isn’t draining properly due to inflammation of the eustachian tube. If the child has significant recurrent infections, tympanostomy tubes may be considered.
Here are two additional examples of acute otitis media.
A presentation on normal ear anatomy is available at Wispr University.

Foreign body – popcorn kernel in ear
A 3-year-old female is brought into the emergency department by her mother. The mother explains that the family had just been enjoying “Friday night movie night” at home when the child began to pull at her ear and complain of pain.
The child has a popcorn kernel in her ear.
Foreign bodies (FB) in pediatric ears and noses are very common. The challenge is being able to see them and to remove them. The WiscMed Wispr is excellent at providing an image of the FB and for documenting the finding in the medical chart. In a 3-year-old pediatric patient, you generally have one “chance” to remove the object before the child will no longer cooperate. If the foreign body can not be removed in the clinical environment, the child will usually need to be sedated; not because removal is painful, but because the child needs to remain still for a successful removal without secondary trauma. In this case, the popcorn kernel was removed in the emergency department under Wispr visualization with a curette. Post removal images were not possible because the child was no longer “cooperative.” The final disposition for the patient included a “Buddy Ball” teddy bear.
WiscMed thanks Dr. Patrick Wolf of The Marshfield Clinic – Rice Lake for the contribution to this case.

Foreign body – hearing aid
A 75-year-old man presents to the VA urgent care clinic with concerns for decreased hearing and discomfort in his right ear. He reports wearing hearing aids. Examination of the right ear reveals this image.
The patient has a foreign body in his ear canal.
The item was easily removed with forceps under direct visualization from the Wispr. On inspection, it turned out to be a piece of the patient’s hearing aid. Retained pieces of hearing aids are a common finding in the outpatient clinic. Irritation of the external auditory canal was noted after removal suggesting that the foreign body had been present for at least several days. The patient did well without further intervention.
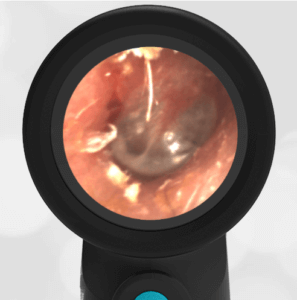
After hearing aid removal

Membrane Rupture-Erosion
A 45-year-old female veteran presents to the VA with concerns for decreased hearing.
The veteran has a subtle tympanic membrane rupture/erosion.

Eardrum rupture/erosion
In addition, it looks like she has had trauma to the ear in the past; the eardrum architecture is distorted and there is evidence of sclerosis. An interesting observation – when the patient performed a Valsalva maneuver, bubbling was evident at the site of the membrane rupture. In a cooperative patient, the Valsalva is helpful in observing the movement of the tympanic membrane without pneumatic otoscopy.

Acute Otitis Media (AOM)
A 10-month-old previously healthy male is brought in by his mother with concern for fever and fussiness. The child continues to take nourishment and has wet diapers. On exam, he is alert, bright-eyed, drooling with a brisk capillary refill. Rhinorrhea is noted, and breath sounds are normal. Ear exam reveals this image.
This child has acute otitis media (AOM).
The tympanic membrane is bulging (donut-shaped) with erythema and loss of bony landmarks. An exam of the other ear reveals the same condition. The child was started on antibiotics for bilateral acute otitis media and did well.
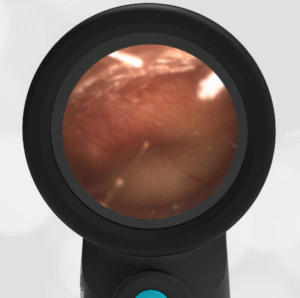
Acute Otitis Media (AOM)
Compare the difference between middle ear effusion (MEE) and AOM.
Below is the actual Wispr video from the examination of the 10-month old. The image above was exported by the Wispr from this video. You can see that these views would have been difficult to achieve with a traditional analog otoscope because of canal size and wax.
Video of Acute Otitis Media
If a child experiences recurrent AOM, ventilation tubes may be indicated. AOM and ventilation tubes can both cause sclerosis.
Available at Wispr University is a presentation on normal ear anatomy.

Foreign body – clear bead in ear
A 3-year old female and her 4-year old brother present to the emergency department with their mother. The mother reports she is sure the 3-year old put something in her brother’s ear. They just came from another emergency department who reported that they could not see anything in the boy’s ear.
There is a clear bead in the ear canal.
You can see the bead channel pointing slightly down. Since putting the bead in her brother’s ear worked so well, the 3-year-old also decided to put a bead in her ear.
Her bead is embedded in ear wax.

Foreign body – bead in sister’s ear
Sharing images with parents and colleagues is a key advantage of the Wispr digital otoscope. The geometry of the speculum with the distal camera allows remarkable access to the ear canal and the tympanic membrane (eardrum). In the case of a pediatric ear foreign body, you generally get one chance to remove the object before the child becomes uncooperative. In the case of the male, the bead was successfully removed with suction in the emergency department. In the case of the female, removal in the emergency department failed. The child had to be sedated for removal by ENT. Removal is not painful, but the child does have to remain still so that secondary trauma to the ear does not occur.
WiscMed has created a presentation on normal ear anatomy that can be viewed here.

Valsalva Maneuver (ear popping)
What causes your ears to “pop” when an airplane descends?
Your ears “pop” when pressure on both sides of the eardrum is suddenly equalized.
The eardrum (tympanic membrane) translates sound waves into motion which is communicated by a chain of bones to the inner ear. For the eardrum to move properly, the pressure on both sides of the eardrum must be the same. The eardrum has two sides. The outer side of the eardrum is exposed to the ear canal and to the “outside.” This is where sound waves enter and where you put the Q-Tips that you shouldn’t. The other side of the eardrum, the middle ear, communicates via the Eustachian tube to the nasal cavity. The Eustachian tube is what keeps the pressure equal on both sides of the eardrum. Although it is called a tube, only part of the Eustachian tube has cartilage. The rest is like a floppy hollow noodle that might stay “closed” because of “stickiness” between the sides of the tube. When the tube is closed, it can not equalize the pressure in the middle ear. This causes the familiar mild ear discomfort during an airplane descent. You may have noticed that this discomfort can be much worse when you have a cold. This is because the inflammation from the viral infection makes the Eustachian tube more likely to be closed.
A commercial airplane flying at 36,000 feet has a cabin pressure of about 6,000 feet. When you descend, the cabin pressure in the aircraft is gradually lowered from 6,000 feet to the altitude of the runway, perhaps 1,000 feet. During this time, your outer ear directly experiences this change in pressure. However, the middle ear can only equalize if the Eustachian tube “communicates” the new pressure via the nasal cavity. You can help this pressure to equalize by moderately forceful attempted exhalation against a closed airway – pinching your nose and holding your mouth shut. When you “pop” your ears, you are actually forcing the Eustachian tube to open (the floppy noodle to expand) to equalize the pressure. In medical terms, popping your ears is called a “Valsalva Maneuver.”
The video below shows a Valsalva Maneuver being performed several times by a healthy individual. You can clearly see the movement of the eardrum when the Valsalva is performed. The movement of the eardrum is due to pressure being increased in the middle ear space via the Eustachian tube.
Valsalva Maneuver
The Valsalva Maneuver might be considered to be the opposite of pneumatic otoscopy. In pneumatic otoscopy, a blast of air is directed at the outer ear to see if there is movement. Movement of the tympanic membrane during pneumatic otoscopy indicates a properly functioning system and likely no infection or perforation. In a cooperative patient, the Valsalva maneuver can be used as a proxy for pneumatic otoscopy.
Extra credit – is this the left ear or the right ear? Find out how to tell here. It’s the left ear.

Tympanic membrane perforation
A 3-year-old male is brought into the emergency department with ear pain. Shortly before arriving he was painting with his older sibling. During the painting activity, some commotion ensued and the child developed acute right ear pain. The examination of the right ear reveals the above image.
The child has a perforation of the tympanic membrane (eardrum) from the pointy end of a paintbrush.
In addition to the circular perforation from the pointy end of the paintbrush, there is significant erythema (redness) and edema (swelling) present that distorts the normal anatomy of the ear. The parents were shown the video from the Wispr and appreciated being able to see the extent of the injury. In addition, the video was uploaded to the EMR system, and Otolaryngology (ENT) was consulted. Usually, eardrum perforations do not require antibiotics. However, in this case, given the possibility of contamination and unknown depth of injury, the child was started on an otic antibiotic drop. The location of the injury (similar in size and location to a tympanostomy tube) suggested that the middle ear ossicles (bones) were spared. The parents were instructed to avoid getting water in the ear until the injury has healed. The child was discharged with antibiotic drops and instructed to follow up in the ENT clinic in a week.
Eardrum perforation video
WiscMed thanks Dr. Josh Ross of the University of Wisconsin BerbeeWalsh Department of Emergency Medicine for this submission.

Extruded tympanostomy tube
A healthy pediatric male patient with a history of otitis media (ear infections) and tympanostomy tubes is seen for a well-child check-up. He has no particular complaints. An image of the right ear reveals this finding.
The child has an extruded tympanostomy tube (ear tube).
Ear tubes are placed in children who have recurrent otitis media (ear infections). The purpose of the ear tubes, sometimes called ventilation tubes, is to equalize the pressure between the outer ear and the middle ear. The tubes also drain fluid from the middle ear. The eustachian tube is usually responsible for drainage and equalizing pressure, but its function can be compromised in case of infection. The tubes are inserted in the eardrum by making a small incision. There are collars on both sides of the tube that hold it in place for about a year. The tubes eventually fall out as shown in this image. The eardrum heals although there is often evidence in the eardrum of their prior placement.
WiscMed thanks Dr. Jitu Modi of the Naval Health Clinic Annapolis for the contribution of this image.

Foreign body – toy gem in ear
A four-year-old male is brought in to the emergency department by his parents because they think he might have something in his ear. The child is not forthcoming with details.
The child has a gem (toy) in his ear.
It is located deep in the external canal and there is no room to maneuver a tool like a Katz extractor around the edge. Because of the smooth nature of the gem, there is also no surface to “grab” for removal. A tactile approach of using a sticky substance at the end of a probe was also unlikely to work because of how tightly the gem was stuck in the canal. Otolaryngology (ENT) was consulted and presented with images of the object from the WiscMed Wispr. The images clearly demonstrated this impacted foreign body, and ENT determined that further attempts in the emergency department were unlikely to be successful. The child was taken to the operating room for uneventful removal of the foreign body under sedation. Removal of the object is not painful, but the child does need to keep still so that secondary trauma to the ear drum does not occur.
Available on Wispr University is our article on normal ear anatomy.

Pars Flaccida Retraction
A 55 year old woman with a history of decreased hearing in her right ear presents for a routine physical exam. She has no new hearing complaints, although she affirms that she has a long history of poor hearing. Examination of her right ear reveals this image.
The patient has retraction and likely erosion of the portion of her tympanic membrane (eardrum) called the pars flaccida.
The pars flaccida is the superior portion of the eardrum and covers portions of the malleus and incus bones. In this image, abnormal anatomy of the pars flaccida is clearly visible with portions of the malleus and incus bones exposed. The portion of the eardrum responsible for the translation of sound waves to mechanical motion, the pars tensa, is intact. The poor hearing is likely due to damage to the articulating surfaces of the malleus, incus, and stapes bones.

Compare the image from this patient with an image of a normal and healthy eardrum. The difference in the pars flaccida is apparent.
If you would like to know more about ear anatomy, please see the WiscMed presentation on normal ear anatomy. It is available at Wispr University.

Exostosis
A 35-year-old male presents to urgent care with gradual onset of left-sided facial pain. The pain is worse with the manipulation of the ear lobe, yawning, and chewing. The examination of the left ear reveals this image.
The patient appears to have exostosis, abnormal growth of bone, in this case in the ear canal. This condition is often associated with people that have extended exposure to cold water – for example, surfers. Exostosis is generally slow to advance and is usually painless. Given that this patient is symptomatic, further investigation is warranted. The next step in evaluation could be either imaging via a CT scan of the temporal bones or a consult with otolaryngology.
WiscMed thanks Dr. Navdeep Gill of Armstrong Urgent Care in Clovis, CA for this interesting image.

Foreign Body: Pinto Bean
A 6-year old previously healthy female presents to the emergency department with her mother. The mother explains that she thinks the child put a bean in her ear two days ago. She was not able to get a good look inside the ear. The child says that her right ear has started to hurt. Examination of the right ear with the Wispr Digital Otoscope reveals this image.
The child has a pinto bean in her ear.
The pinto bean is completely occluding the external auditory canal and no portion of the eardrum is visible. Fortunately, the pinto bean was quite superficial and was easily removed under direct visualization using tweezers.
After removal, a minor abrasion of the posterior external auditory canal was noted as shown in the image below. Topical medications were considered but believed to be unnecessary. The child did well without further intervention.
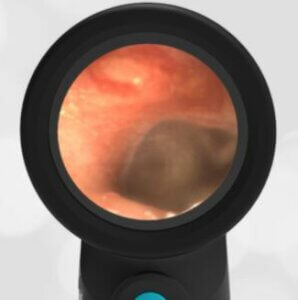
Pinto Bean Removed – Minor Abrasion

Tympanostomy Tubes
A 7-year male patient is brought into the emergency department by his mother. The mother explains that the child has a history of ear infections and recently had “ear tubes” placed. She is concerned because the child says his ears “feel funny.” Otherwise, the child has no complaints. The mother would like the child “checked-out” because of his history of ear infections. Examination of his ears with the Wispr Digital Otoscope reveal these images.
The images show tympanostomy tubes (ear tubes).
Both tubes (the blue circles) are well-placed and appear patent. The ears are otherwise normal. The eardrum is not bulging, there is no erythema (redness) and the bony landmarks are normal. On close inspection, you can see exquisite vasculature associated with the malleus. This is a normal finding.
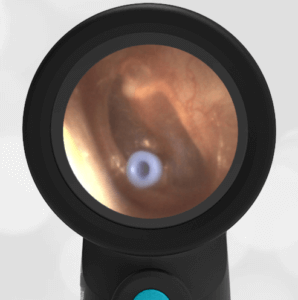
Left Ear – Tympanostomy Tube
Pressure in the middle ear is regulated by the eustachian tube that connects the oral cavity to the middle ear. Adults are accustomed to equalizing the pressure in their ear (for example on an airplane in descent) by increasing pressure in their mouth. In children, the developing anatomy of the eustachian tube may not be straight enough to accommodate the relief of pressure in the middle ear. This can lead to recurrent infections and discomfort. Ear tubes, sometimes called ventilation tubes, are placed to help with this condition until their anatomy matures. The tubes relieve the pressure in the middle ear by communicating directly with the “outside.” The tubes typically fall out on their own over the course of months to a year. There will often be evidence of prior tympanostomy tubes.
At Wispr University, you will find an article on normal ear anatomy.

Myringosclerosis (sclerosis)
A previously healthy 30-year-old female presents to primary care for a routine physical exam. She has no complaints. Examination of her right ear with the Wispr Digital Otoscope reveals this image.
The patient has myringosclerosis (sclerosis) of the eardrum.
This is the white area highlighted in this image.
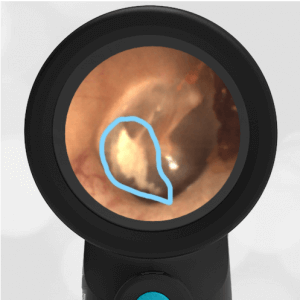
Highlighted Sclerosis
Sclerosis is a localized hardening of the tympanic membrane. It can be caused by a history of acute otitis media (AOM) and it is very commonly associated with a prior history of tympanostomy tube (ear tube) placement. There is generally no consequence to the sclerosis. Hearing is not usually materially compromised.
Here is a comparison of a healthy and a sclerosed right ear.
At Wispr University you can see a presentation on normal ear anatomy.

Which Ear?
A healthy 23-year-old female presents for a routine sports physical exam. This image is obtained Wispr Digital Otoscope. Unfortunately, the examiner forgot to make note of which ear the image is from for the medical record. How can you tell which ear the image is from? This is one of our favorite questions to ask learners because the answer is simple and useful.
This image is from the right ear.
It’s easy to tell because of the orientation of the malleus bone. The malleus points like an arrow towards the face of the patient.

A prominent feature of the ear exam is the presence of the malleus bone. This is the first of three bones in the middle ear that communicates the movements of the eardrum, from sound waves to the inner ear. The formal names of the three bones are malleus, incus, and stapes. These are commonly referred to as “hammer, anvil, and stirrup.” Conveniently, the malleus is like an orientation compass for the examiner in an ear with normal anatomy.
Compare the right ear and the left ear taken from the same patient.

Foreign Body: (Bead) In Nose
A 6-year old female presents to the emergency department with a foreign body in her nose. Her mother reports that the child had been playing with beads and decided that it would be a good idea to put the bead in her nose. The mother attempted to remove the bead without success. This was followed by a trip to urgent care where they were able to see the bead with an analog otoscope, but were unable to remove the foreign body. The family was sent to the emergency department. Examination of the nostril with the Wispr Digital Otoscope revealed this image.
The child has a bead in her nose.
A benefit of the Wispr is the ability to easily share with the parents the location of the foreign body and to discuss removal options. A resident physician attempted to remove the bead with a Katz extractor. A Katz extractor is a small tube with a balloon at the end that can be passed beyond a foreign body, inflated, and then extracted to bring the foreign object out. Unfortunately, the first attempt was not successful and the child was no longer “cooperative.”
After sedating the child, the bead was uneventfully removed using the extractor under direct visualization from the Wispr. A key benefit of the Wispr is its anti-fog coating that allows for a clear image even in a high-humidity environment like the nose. After removal, minor irritation to the nasal mucosal was noted that was not felt to need additional treatment.
Here is the video from the Wispr of the bead in the nose.
Although the Wispr otoscope is optimized for use in the ear canal, it can be useful in examining both the nose and mouth.
WiscMed thanks Dr. Michael Kim of the University of Wisconsin BerbeeWalsh Department of Emergency Medicine for the submission of this interesting image.

Bullous Myringitis
A 7-year old female is brought in to the emergency department with concerns of right ear pain and symptoms for one day. The child has a history of ear infections. The discomfort associated with this episode seems worse. The mother has tried alternating ibuprofen and acetaminophen, but it has not significantly helped the symptoms. The examination reveals an afebrile child, crying and rocking on the gurney, and holding her right ear. This image is obtained with the Wispr Digital Otoscope.
The child has bullous myringitis.
Bullous myringitis is an inflammation of the tympanic membrane (eardrum) that produces blisters. It occurs as part of the spectrum of acute otitis media (ear infection). It can be a dramatic finding in an uncomfortable child.
Historically, bullous myringitis was thought to be caused by Mycoplasma pneumoniae. However, as Mellick(1) shows in his letter, it is a component of severe AOM whose underlying cause may be a number of infectious agents.
Treatment is focused on providing pain relief along with treating the underlying infection. An anesthetic such as topical lidocaine can be introduced in the ear canal to provide timely pain relief. Treatment of the underlying infection is the same as for acute otitis media.
WiscMed thanks Dr. Andrew Schuman of medgizmos for the submission of this image.
(1) Mellick and Verma, Letter, Pediatric Emergency Care, Volume 26, Number 12, December 2010

Otitis Media With Effusion
A mother brings in her 7-year-old son for fever and ear pain. The mother reports the child has had viral symptoms including fever to 101 F, cough, and runny nose for the past 3 days. Earlier in the day, the child began to complain of left ear pain. Examination of the left ear with the Wispr Digital Otoscope reveals this image.
The child has otitis media with effusion (OME).
OME is notable for fluid behind the eardrum (circled area), without other signs of infection such as bulging of the eardrum or loss of bony landmarks. Compare the OME image with acute otitis media (AOM) below. It is easy to confuse OME with AOM if you do not obtain a good view of the eardrum.

Otitis Media with Effusion (OME)

Acute Otitis Media (AOM)
View Additional Cases
- History of Tympanostomy Tubes – November 21, 2024
- Hemotympanum – November 14, 2024
- Spring In Mouth – November 7, 2024
- Primary Blast Injury – October 31, 2024
- Ant in Ear Canal – October 24, 2024
- Otitis Media with Effusion – October 17, 2024
- Bullous Myringitis – October 10, 2024
- TMJ Compression of External Ear Canal – October 3, 2024
- Tick in Ear – September 26, 2024
- Acute Otitis Media – September 19, 2024
- Myringosclerosis – September 12, 2024
- Mud Spots (REMEMP) – September 5, 2024
- Ear Wax – August 29, 2024
- Bilateral Osteoma – August 22, 2024
- Foreign Body – August 15, 2024
- Ant in Ear – August 8, 2024
- Eustachian Tube Shadow – August 1, 2024
- Chronic Otitis Media with Effusion – July 25, 2024
- Osteoma – July 18, 2024
- Acute Otitis Media with Penicillin Allergy – July 11, 2024
- Retraction – June 27, 2024
- Myringoplasty with Valsalva – June 20, 2024
- Epistaxis – June 13, 2024
- Perforation – June 6, 2024
- Bilateral AOM – May 30, 2024
- Myringoplasty – May 23, 2024
- Nasal Septal Hematoma – May 16, 2024
- Osteoma – May 9, 2024
- Periosteal Abscess – May 2, 2024
- Resistant Acute Otitis Media – April 25, 2024
- Pars Flaccida Retraction – April 18, 2024
- Acute Otitis Media – April 11, 2024
- Myringosclerosis and Myringoplasty – April 4, 2024
- Recent Acute Otitis Media – March 28, 2024
- Acute Otitis Media – March 21, 2024
- Bilateral Acute Otitis Media – March 14, 2024
- Foreign Body – March 7, 2024
- Otitis Media with Effusion – February 29, 2024
- Bullous Myringitis – February 22, 2024
- Otitis Media with Effusion – February 15, 2024
- Mucopurulence – February 8, 2024
- Acute Otitis Media – Feb 1, 2024
- External Ear Canal Bleeding – January 25, 2024
- Extruded Ventilation Tube – January 18, 2024
- Hemotympanum – January 11, 2024
- Otitis Media or Externa – December 21, 2023
- Normal Ear Drum Features – December 14, 2023
- Cotton Swab Foreign Body – December 7, 2023
- Middle Ear Effusion – November 30, 2023
- Bullous Myringitis – November 16, 2023
- New Ear Tubes – November 9, 2023
- Ear Trauma – November 2, 2023
- Ear Canal Osteoma – October 26, 2023
- Bilateral AOM – October 19, 2023
- Acute Otitis Media – October 5, 2023
- Ear Pain – September 28, 2023
- Ear Trauma – September 21, 2023
- Otitis Media with Effusion – September 14, 2023
- Ear Drum Lesion – Sept 7, 2023
- Acute Otitis Media – August 31, 2023
- Myringosclerosis – August 24, 2023
- Otitis Media with Effusion – August 17, 2023
- Nasal Foreign Object – August 10, 2023
- Ear Canal Trauma – August 3, 2023
- Foam in Ear Canal – July 27, 2023
- Tympanostomy Tube – July 20, 2023
- Bullous Myringitis – July 13, 2023
- Ear Canal Polyp – June 29, 2023
- Acute Otitis Media – June 22, 2023
- Foreign Object – Eraser Tip – June 15, 2023
- Waxy Ear – June 8, 2023
- Foreign Body? – June 1, 2023
- Incudomalleolar Joint – May 25, 2023
- Middle Ear Effusion – May 18, 2023
- Exostosis – May 11, 2023
- Wax Annulus – May 4, 2023
- Mild Bulging AOM – April 27, 2023
- Cholesteatoma – April 20, 2023
- Resolving AOM – April 13, 2023
- Chronic Changes – April 6, 2023
- Healthy Tympanic Membrane – March 30, 2023
- Blocked Ear Tube with AOM – March 23, 2023
- Acute Otitis Media with Scant Erythema
- Middle Ear Effusion with Cerumen
- Mastoiditis
- Visual Ear Diagnosis
- Ear Canal Trauma
- Otitis Media with Effusion (OME)
- Resolving Acute Otitis Media
- Seed in Ear
- Myringoplasty
- Ventilation Tube
- Middle Ear Effusion
- Hemorrhagic Bullae
- Normal Ear
- Otitis Media with Effusion
- Neonatal Acute Otitis Media
- Bullous Myringitis
- Otitis Externa
- Diffuse Sclerosis
- Bleeding Ear Canal
- Shagrination or “Cobble Stoning”
- Middle Ear Effusion
- Bullous Myringitis
- Bilateral Acute Otitis Media (AOM)
- Fibrous disk
- Erythema
- Acute Otitis Media (AOM)
- Developing Acute Otitis Media (AOM)
- Myringosclerosis
- Tympanostomy or Ventilation Tubes
- Acute Otitis Media (AOM)
- Retained Hearing Aid Tip
- Bullous Myringitis vs Cholesteatoma Pearls
- Normal Ear Drum Anatomy
- Bulging Pars Flaccida
- Acute Otitis Media (AOM)
- Eardrum Retraction
- Localized Thickening Of The Tympanic Membrane (Eardrum)
- Bones Of The Middle Ear
- Significant Exostosis
- Exostosis
- Middle Ear Effusion
- Acute Otitis Media
- Extruded Ventilation Tube
- Hemotympanum
- AOM with Shagrination
- Retraction Pocket
- Mild Bulging of the Eardrum
- Tympanic Perforation
- Fibrous Disk
- Foreign Body – fly in ear
- Foreign Body – Pencil Tip
- Bullous Myringitis
- Quadrants of the Tympanic Membrane
- Ear Ventilation Tube
- Resolving Acute Otitis Media
- Seborrheic Dermatitis
- Otitis Media with Effusion (OME)
- Progression to AOM
- Foreign Body – Tic Tac
- Acute Otitis Media (AOM)
- Significant Cerumen
- Myringosclerosis
- Acute Otitis Media (AOM)
- Stapes Bone
- Foreign Body – Ear Bud
- Shagrination or “Cobble Stoning”
- Extruded and Encrusted Ventilation Tube
- Perforation of the Tympanic Membrane
- Middle Ear Effusion
- Foreign Body – Earring
- Otitis Externa and Mild Acute Otitis Media
- Acute Otitis Media
- Foreign Body – Hearing aid tip
- Bilateral Hemotympanum
- Acute Otitis Media
- Mild Acute Otitis Media (AOM)
- Hemorrhagic Bulla
- Otitis Externa
- Middle Ear Effusion
- Malleus and Components
- Pulsatile Tympanic Membrane Perforation with Effusion
- Bullous Myringitis
- Middle Ear Effusion
- Foreign Body
- Acute Otitis Media
- Tympanic Membrane Defect with Middle Ear Discharge
- What is Your Advice?
- Hair in View
- Acute Otitis Media
- Initiate Antibiotics?
- Worried Parents
- Perforation of the Tympanic Membrane
- Otitis Media
- Foreign Body – Spider in Ear
- Chorda Tympani Nerve
- Normal Left Ear Drum
- Otoscope Grip Preference
- Perforation of the Tympanic Membrane
- Otitis Media with Effusion
- Pars Tensa and Pars Flaccida
- Eustachian Tube Dysfunction
- Cartilage Lesion
- Desquamated Keratin
- Middle ear effusion
- Foreign body – bead in ear
- Complete ear wax (cerumen) obstruction
- Prominent Vasculature
- Do you agree with the diagnosis of acute otitis media?
- Acute Otitis Media (AOM)
- Foreign body – popcorn kernel in ear
- Foreign body – hearing aid
- Membrane Rupture/Erosion
- Acute Otitis Media (AOM)
- Foreign body – clear bead in ear
- Valsalva Maneuver (ear popping)
- Tympanic membrane perforation
- Extruded tympanostomy tube
- Foreign body – toy gem in ear
- Pars Flaccida Retraction
- Exostosis
- Foreign body – pinto bean in ear
- Tympanostomy Tubes (ear tubes)
- Myringosclerosis (sclerosis)
- Which Ear?
- Foreign Body (Bead) In Nose
- Bullous Myringitis
- Otitis Media With Effusion