5-year-old with Ear Pain
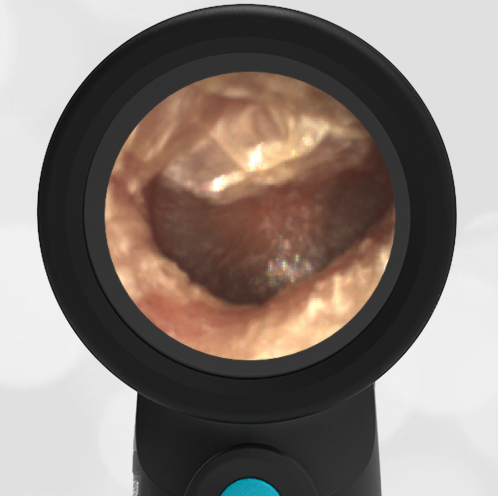
A 5-year-old child presented to the emergency department (ED) with two days of right-sided ear pain. His mother reported her son had a history of otitis externa, and she was concerned this may be the cause of his pain. She noted he complained of discomfort and had yellowish drainage from the ear approximately two days prior to the visit. She began using “drying drops” that had been recommended by his ENT doctor following a past evaluation. He denied experiencing itchiness in the ear and stated that the pain had significantly worsened over the past two days. On PE, the child was uncomfortable but afebrile. His external ear demonstrated normal position without posterior auricular erythema or warmth. He reported discomfort with the manipulation of the external ear. His Wispr digital otoscope exam is attached below.
Which of the following is/are true of this child’s clinical presentation?
A. He has signs and symptoms of acute otomastoiditis
B. His tympanic membrane (TM) demonstrates shagrination
C. He has signs and symptoms of acute otitis externa (AOE)
D. B & C

The child in this scenario presented with a mixed picture of external ear canal (EAC) inflammation and an abnormal appearance of the tympanic membrane (TM, “eardrum”). Manipulation of his external ear caused discomfort, as would be expected with acute otitis externa (AOE), and he has purulence in his EAC. His TM has the cobblestoned finding of “shagrination” but is not bulging—on the contrary, the posterior superior quadrant has a “deflated” appearance. He had no mastoid or posterior auricular findings of tenderness, warmth, swelling, or erythema to suggest otomastoiditis.
His mother reported a prior history of several episodes of AOE, and he had been evaluated by a Pediatric ENT specialist who recommended a drying agent in the ear canal. Upon review of his chart, his bouts of AOE were not felt to be secondary to eczema, canal injury, or excessive cerumen. And while he enjoyed swimming, the episodes were not always associated with pool time. His TM demonstrated cobblestoning (shagrination) without bulging. One hypothesis is that this TM finding occurs following bulging and perhaps indicates a resolving acute otitis media (AOM). Notably, AOE may occur concomitant with AOM (noting that Streptococcus pneumoniae can cause both conditions) or secondary to AOM with rupture when the purulent drainage causes inflammation to the EAC. The clinician in this scenario chose to treat the AOE with topical antibiotic drops to cover for the two most common pathogens—Pseudomonas aeruginosa and Staphylococcus aureus--and scheduled ibuprofen as recommended by Otolaryngologic practice guidelines.
Contact was continued with the family, and arrangements were made to re-evaluate the child in two days. At that time, they reported he no longer required ibuprofen. His Wispr exam for this visit is attached below—while he continued to have EAC purulence and shagrination, his overall improvement in symptoms was felt to indicate clinical response to the topical antibiotic. It is also notable that he had not developed bulging of the TM, perhaps supporting the hypothesis that shagrination occurs on the continuum of resolution of AOM.
Follow Up Image:

References:


