Developing Acute Otitis Media (AOM)
A 4-year-old female presents to the emergency department (ED) for evaluation of fever and ear pain. Her parents note she has had mild congestion for the past week but otherwise was well until that evening. Shortly after going to bed, the child woke with right ear pain. The parents gave her a dose of acetaminophen and put her back in bed. However, less than an hour later the child woke with worsening pain so she was brought in for concerns of an ear infection.
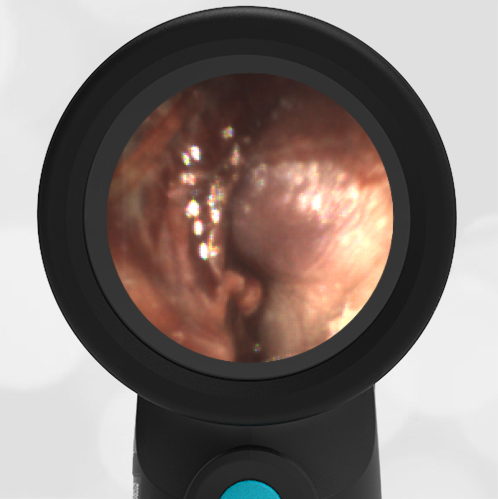
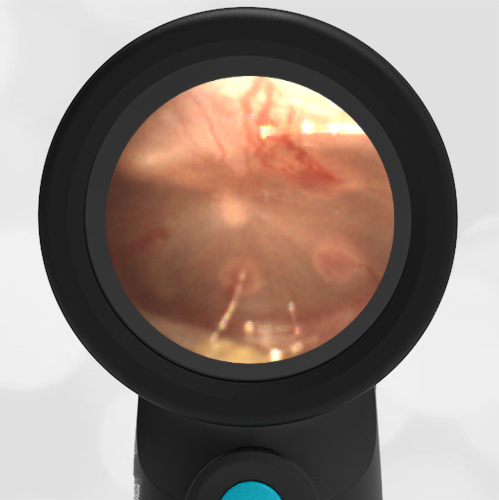
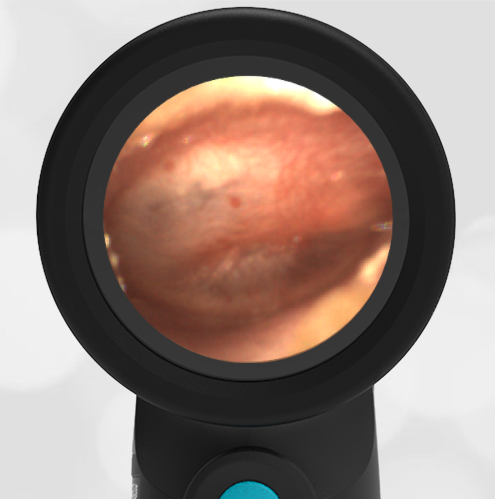
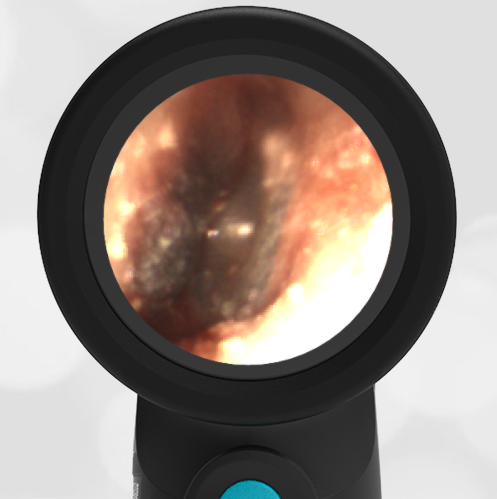
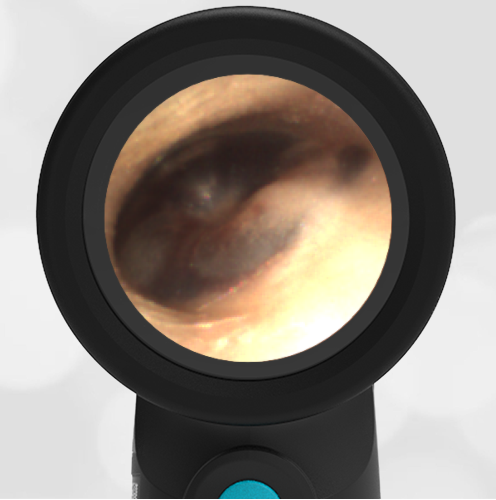
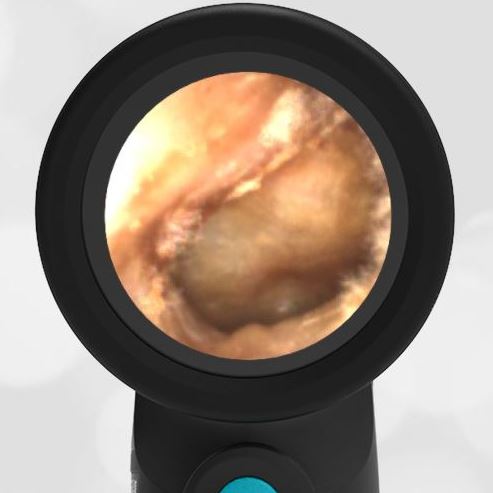
In the ED, the child is well-appearing and afebrile. There is mild congestion with clear rhinorrhea. The Wispr exam is shown here. Based on the AAP otitis media clinical practice guideline, how should this be managed?
The child likely has developing acute otitis media (AOM) and antibiotics should be considered.

This child’s ear exam demonstrates mild bulging, or “fullness”. The notable characteristics are the indistinct malleus (due to the bulging in the pars flaccida) superiorly and a shallow dimpling in the center of her tympanic membrane. Mild bulging can be caused by other conditions such as fever, crying, Eustachian tube dysfunction, and resolving otitis media. To help differentiate (likely early) acute otitis media demonstrating mild bulging from these other conditions, the 2013 AAP Clinical Practice Guideline on Diagnosis and Management of AOM recommends additional signs (intense erythema) and symptoms (pain) ought to be present. The presence of such additional findings increases the likelihood of AOM significantly.
The current patient demonstrates pain as well as injection of the tympanic membrane (TM). Given this clinical picture, one could reasonably elect to treat with antibiotics. In this child, we elected to treat her pain with topical anesthetic and provide a prescription to be filled the following day if the pain persisted. The rationale for this approach is that we felt managing the child’s late-night pain was more important than immediate initiation of antibiotics. Also, while there is certainly prominence of the vasculature to her TM, we did not feel this raised to the level of “distinct erythema” referenced in the AAP guideline. Thus, we also felt waiting a short period to see if symptoms more strongly indicated an evolving AOM was appropriate.
Upon follow-up call the following evening, the family reportedly filled their prescription shortly before dinnertime.
Here is the complete video exam:
Complete exam video