Neonatal Acute Otitis Media
A 6-week-old male infant presents to the Emergency Department (ED) for congestion and fussiness. He was born at full term without complications and had been doing very well despite a recent onset of cough. However, earlier that evening he developed a fever to 101.5, and, after calling their pediatrician’s nursing line, the family was directed to the ED for evaluation. Upon arrival, the child had a temperature of 101.2 F, RR 52, HR 160, and POx 96% on room air.
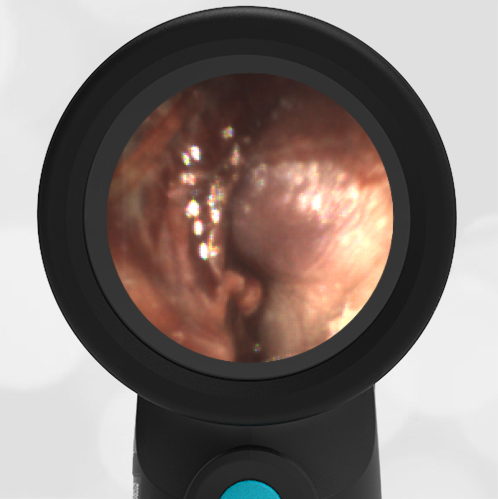
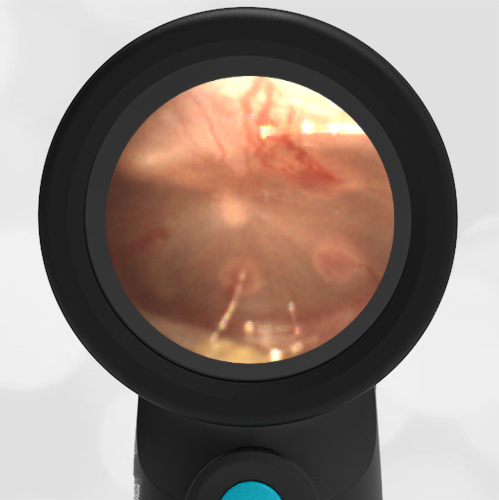
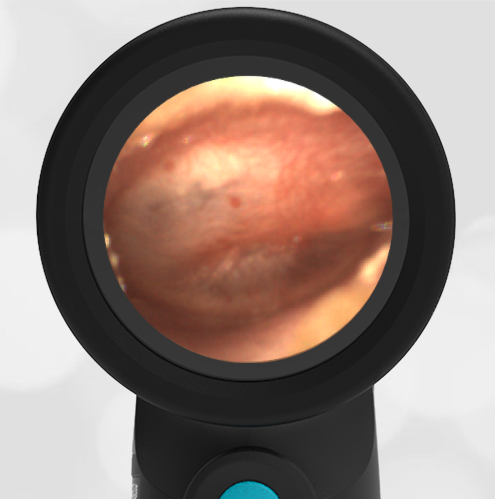
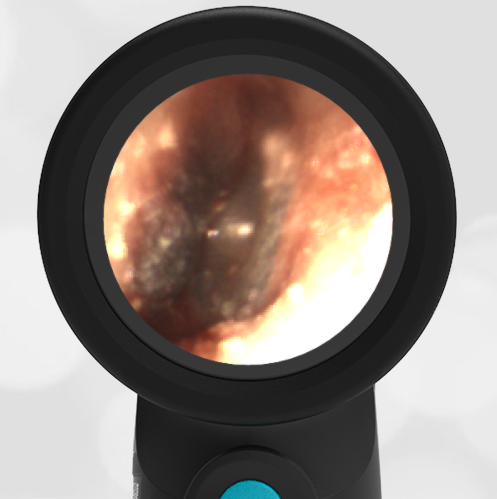
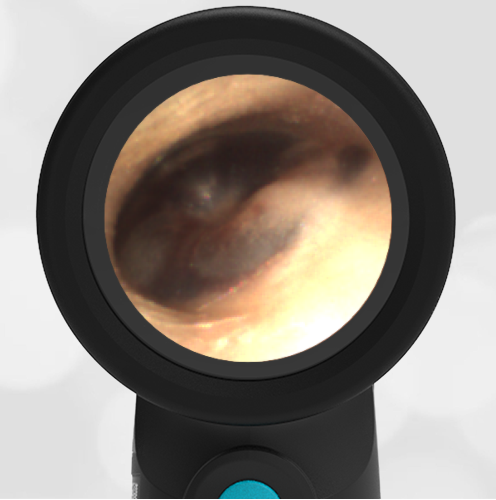
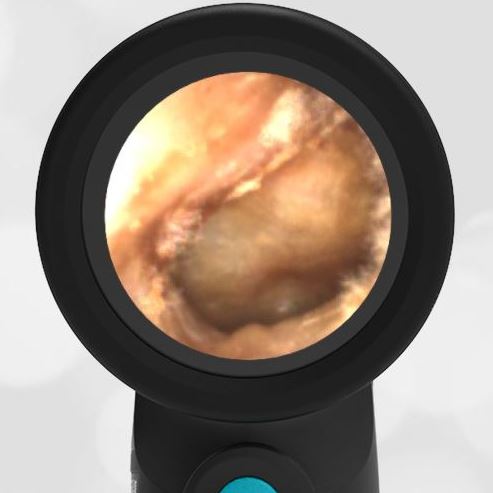
He was well-appearing with very mild retractions and occasional wheezes. His Wispr exam is shown here. The remainder of his examination was non-focal. The infant received a dose of acetaminophen and nasal suctioning which improved his work of breathing and decreased his RR to 45. A respiratory panel was collected which resulted positive for the respiratory syncytial virus (RSV). His urinalysis was negative (culture sent) and a complete blood count (CBC) demonstrated a white blood count of 6,000 with less than 5% bands.
What is your diagnosis and treatment?
The infant has laboratory-proven RSV with clinical evidence of acute otitis media (AOM).

The infant in this case has a clear case of RSV bronchiolitis, a condition that has spread across the pediatric landscape like wildfire in the fall of 2022. In addition to his respiratory illness, the infant also has strong evidence of acute otitis media (AOM) with moderate bulging, loss of landmarks, and a purulent effusion noted on his Wispr exam. The association between RSV bronchiolitis and AOM is well-described (1-3), so perhaps it is not surprising there has also been a significant jump in the diagnosis this season—one that may be contributing to amoxicillin shortages seen in certain parts of the country (4). The causative pathogens in infants are felt to be the same as in older children, however many clinicians rightfully exercise caution with diagnosing AOM in the very young infant out of fear of missing a serious bacterial illness (SBI) (5,6).
In his 2018 Pediatric EM Morsels article, Dr. Sean Fox provides an eloquent and succinct discussion of the pitfalls associated with neonatal AOM (5,6). Major challenges include 1. Adequately visualizing and appreciating the anatomic uniqueness of the TM in infants, and 2. Should AOM be considered an SBI requiring septic work-up in infants? While no gold standard for evaluation exists, interpretation of the available evidence suggests following the typical risk stratification for infants older than 28 days—usually including CBC, urinalysis, and (when appropriate) respiratory viral swabs. For the well-appearing infant with low-risk stratification, management with an oral antibiotic and close follow-up is reasonable. However, for neonates less than 28 days of age with fever, this approach may not be advisable as it is unclear if AOM remains localized in this very immature cohort (6). The patient in our case was started on high-dose amoxicillin and at follow-up appeared to be doing very well and was no longer febrile.
Prior to this case, the author (with over 20 years of pediatric ear exams), had never confidently observed AOM in such a young child. Similar to the experience described in Dr. Fox’s discussion, I will admit to being slightly dubious when I am told that a neonate has been diagnosed with AOM. However, as observed in this case, digital otoscopy has once again helped address the major challenge of visualizing the TM, provided much greater diagnostic certainty, and may offer a tool for future research on AOM in this very young cohort.
Here is the complete video of the exam:
Complete exam video
References
1. Risk of acute otitis media in relation to acute bronchiolitis in children
Gomaa MA, Galal O, Mahmoud MS.Int J Pediatr Otorhinolaryngol. 2012 Jan;76(1):49-51.
2. Acuteotitismedia in children with bronchiolitis
Andrade MA, Hoberman A, Glustein J, Paradise JL, Wald ER.Pediatrics. 1998 Apr;101(4 Pt 1):617-9.
3. The clinical course of bronchiolitis associated with acute otitis media
Shazberg G, Revel-Vilk S, Shoseyov D, Ben-Ami A, Klar A, Hurvitz H.Arch Dis Child. 2000 Oct;83(4):317-9.
4. https://www.livescience.com/amoxicillin-shortage-explained
5. https://pedemmorsels.com/neonatal-acute-otitis-media/
Sakran W, Makary H, Colodner R, Ashkenazi D, Rakover Y, Halevy R, Koren A.Int J Pediatr Otorhinolaryngol. 2006 Apr;70(4):613-7